Let’s be real: measles is one of those words that makes any parent’s stomach drop. But here’s the deal—you don’t need a color-coded panic plan. You just need the facts, the symptoms to watch for, and a clear plan if you suspect it.
Let’s walk through exactly what you need to know to keep your family safe and (reasonably) calm.
What Is Measles (Rubeola) in Kids?
Measles (also called rubeola) is not some vague old-timey illness—it’s a real, highly contagious viral infection that can cause serious complications in children. Here’s why you want to know about it.
Why Parents Should Care About Measles
Measles is more than “just a rash.” It can cause pneumonia, brain swelling (encephalitis), dehydration, and, in severe cases, death. Kids under 5 are particularly vulnerable.
“It’s so important for parents to recognize measles early,” says Jessica Kimmes, a Poppins pediatric nurse practitioner. “It spreads incredibly easily, and catching it early helps reduce exposure to others—especially babies and immunocompromised individuals.”
How Measles Spreads So Easily
Measles is one of the most contagious viruses out there. It spreads through the air when an infected person coughs or sneezes, and the virus can linger in the air for up to two hours. Even brief contact can cause infection if your child isn’t immune.
Measles Symptoms in Children
This is where being prepared really matters. Measles isn’t subtle—it has a classic progression of symptoms that make it recognizable once you know what to watch for. The tricky part is that the early signs can look like a common cold or flu. Here’s how to tell the difference and when to be extra cautious.
The 3 Big “C’s” of Measles to Watch For
Before the telltale measles rash appears, there are three classic early warning signs that doctors look for—known as the “3 C’s.” Recognizing these symptoms early can help you spot measles sooner and know when to call your provider. These symptoms often show up a few days before the rash, making them important clues for parents:
- Cough: Often dry and hacking. Not just a mild tickle—it can be persistent and uncomfortable for kids.
- Coryza (aka runny nose): Coryza is a fancy word for a runny nose. Think of it as that constant drip you can’t seem to wipe away.
- Conjunctivitis: Red, watery eyes that can be sensitive to light, sometimes described as “pink eye”–like.
These “3 C’s”, along with a lack of immunity or known exposure, are the classic warning signs that set measles apart from other common viruses.
Parent tip: Don’t dismiss them if you know there’s been measles exposure in your community. Early recognition is key to preventing spread.
Fever and How Long It Lasts
Fever is another one of the early (and most reliable) signs of measles, often appearing before the rash and other classic symptoms. Unlike the low-grade fevers that sometimes come with mild colds, measles usually causes a higher and more stubborn fever.
It’s important for parents to know what to expect and when to worry.
- Typical pattern: High fever, often peaking around 104°F (40°C).
- Duration: Usually lasts several days and may coincide with worsening respiratory symptoms.
“Persistent high fever is a red flag,” says Kimmes. “It’s one of the key signs to monitor if you suspect measles.”
If your child’s fever won’t come down with medication or keeps climbing, call your pediatrician or contact your Poppins care team right away.
Koplik Spots: The Tell-Tale Mouth Sign
Koplik spots are one of the most distinctive early signs of measles, often helping doctors confirm the diagnosis even before the classic rash appears. While they can be tricky for parents to spot at home, knowing what to look for can give you an important clue if you suspect measles. These tiny spots are a classic diagnostic feature that providers check for during exams.
- What they look like: Small, white or bluish-white spots with a red base, appearing on the inside of the cheeks.
- Timing: Usually show up 1–2 days before the rash.
- Why they matter: They’re considered a hallmark sign of measles but can be hard for parents to see without a good look in the mouth.
If you spot them, let your pediatrician know right away.
The Classic Measles Rash
The rash is the most recognizable sign of measles—and by the time it shows up, your child has already been contagious for days.
- Timing: Typically appears 3–5 days after the first symptoms (fever, cough, runny nose, conjunctivitis).
- Appearance: Starts on the face at the hairline and spreads downward to the neck, trunk, arms, legs, and feet.
- Pattern: Begins as small red spots that merge into larger, blotchy patches.
- Healing: As the rash fades, it can leave behind a brownish discoloration and sometimes mild peeling.
Parent tip: Track when the rash appears and how it spreads. This info helps your doctor confirm the diagnosis.
Other Symptoms Like Diarrhea and Fatigue
Measles doesn’t just stop at cough and rash. Some kids have other symptoms that can be easy to overlook but still need attention:
- Diarrhea: Can lead to dehydration, especially in babies and toddlers.
- Marked fatigue: Kids might seem unusually tired, cranky, or just not themselves.
- Irritability: Some kids become hard to comfort as they feel worse.
Parent tip: Watch for dehydration signs like fewer wet diapers, dry mouth, or no tears when crying.
Bottom line: If you know there’s a risk of exposure and your child shows these symptoms, don’t wait—call your pediatrician or use Poppins for guidance. Early action helps protect your child and those around you.
How Long Before Symptoms Appear?
One of the most confusing—and frankly, nerve-wracking—parts of measles is the timing. Kids can seem perfectly fine before suddenly showing symptoms, and they can spread the virus even before you know they’re sick. Understanding the timeline helps you know when to watch carefully after possible exposure and when to take action.
Measles Incubation Period (7–14 Days)
After your child is exposed to measles, there’s typically an incubation period of about 7–14 days before any symptoms appear.
- What this means for parents: Your child might seem completely healthy during this window. No fever, no cough, nothing that screams “measles.”
- Why it matters: Even though they look fine at first, symptoms can appear suddenly—so it’s important to keep track of any known exposures and monitor carefully during this time.
Typical progression includes:
- Early symptoms like fever, cough, runny nose, and conjunctivitis showing up first (often around day 10–12 after exposure).
- Rash typically develops a few days after the early symptoms begin.
“We tell parents to think about a two-week window,” says Kimmes. “If there was an exposure, be extra alert for any symptoms during that time.”
When Is a Child Contagious? (The “4 & 4 Rule”)
This is one of the most important things for parents to know—and one of the reasons measles spreads so quickly in schools, daycares, and households.
- Contagious period: Kids with measles are contagious for 4 days before the rash appears and 4 days after it starts.
- Why this matters: Your child can spread the virus before you even realize they have measles. Even brief contact with an infected child can be enough to pass it on.
This “4 & 4 rule” is the reason health departments often recommend quarantine for exposed, unimmunized kids—even if they seem healthy. It helps prevent spreading the virus to babies, pregnant people, and immunocompromised individuals who can get seriously ill.
Measles Timeline Table
Here’s what they typical timeline from measles exposure to rash looks like:
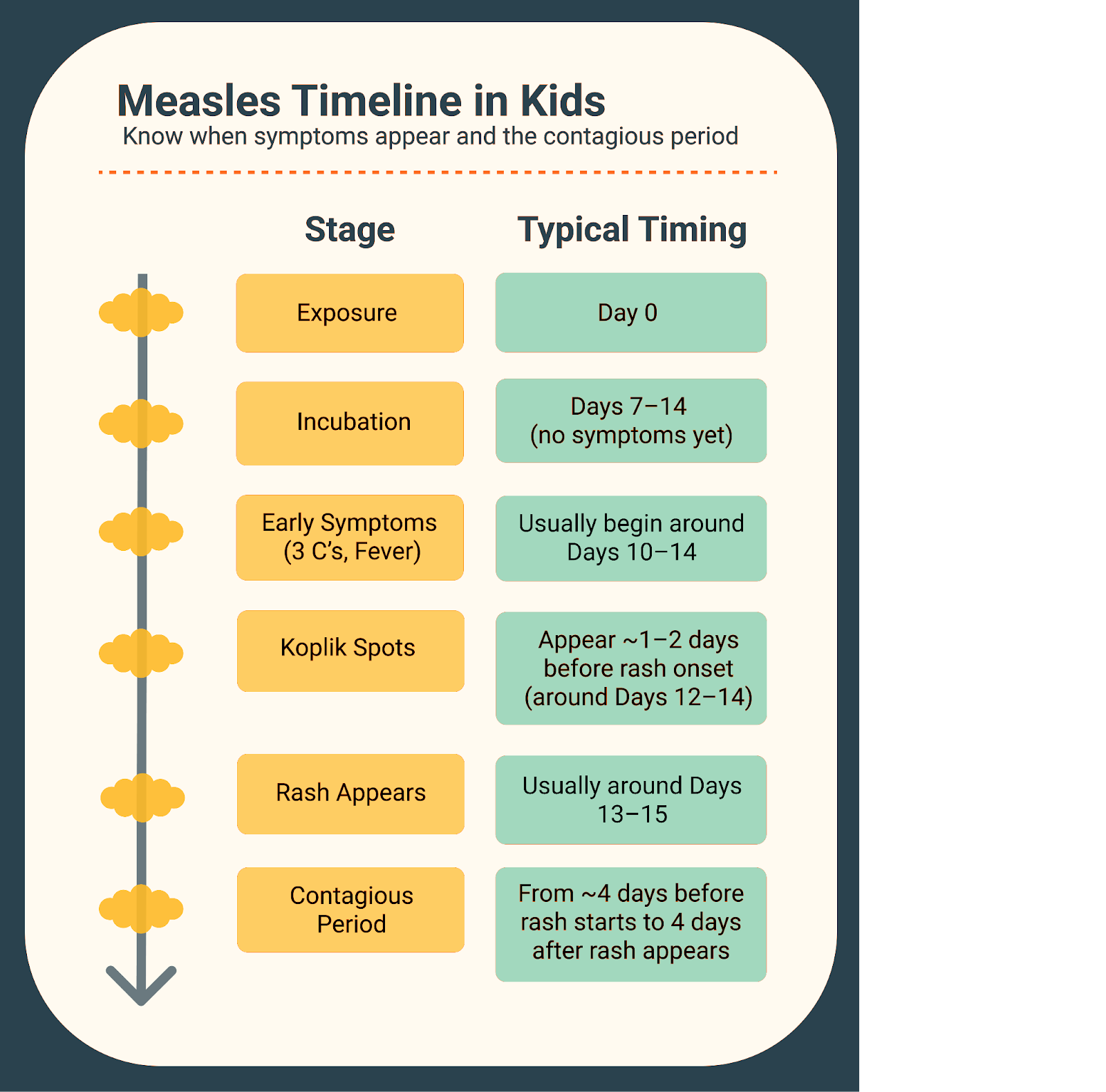
Bottom line? Know the timeline. Be ready to watch carefully for symptoms for two weeks after exposure, and understand that contagiousness can begin before any rash shows up. This awareness is key to stopping outbreaks in their tracks.
Measles Risk Factors for Kids
Not every child has the same risk when it comes to measles. Knowing who’s most vulnerable helps you make smart choices about vaccination, travel, and limiting exposure. Let’s walk through the key factors parents should keep in mind.
Vaccine Status and Immunity
The biggest risk factor is whether your child is vaccinated. Kids who haven’t received the MMR (measles, mumps, rubella) vaccine—or who haven’t finished the full two-dose series—are at much higher risk of getting sick if exposed.
Two vaccine doses offer strong, long-lasting protection with 97% effectiveness against measles. Even one dose is about 93% effective at preventing measles infection overall.
“Vaccination is the single most effective way to prevent measles,” emphasizes Kimmes. “It’s about protecting your own child and the people around them.”
Travel Risks (Domestic and International)
Measles can show up in any community, but travel adds an extra layer of risk.
- International travel: Many countries still have active measles transmission. A single trip can lead to exposure.
- Domestic travel: Outbreaks sometimes happen in specific regions or communities.
Before traveling, check travel advisories, make sure your child is fully vaccinated if eligible, and talk to your pediatrician about any added precautions.
Exposure to At-Risk Groups
Even if your child handles measles with mild symptoms, they could easily pass it to someone far more vulnerable.
Measles is one of the most contagious viruses we know. A single infected person can spread it to 9 out of 10 unvaccinated people they’re near. That’s why preventing its spread isn’t just about protecting your own child—it’s about protecting others in your family and community who might not have the same level of defense. Some people are at much higher risk of serious, even life-threatening, complications if they catch measles.
Measles is especially dangerous for:
- Pregnant individuals: Infection during pregnancy can lead to serious complications for both parent and baby.
- Babies under 12 months: Too young for routine MMR vaccination, leaving them unprotected.
- Immunocompromised people: Those with weakened immune systems (from conditions or treatments) can have life-threatening complications from measles.
If your child has symptoms or known exposure, limit contact with these groups.
Bottom line: Knowing these risk factors isn’t about adding stress—it’s about giving you the knowledge to make safe, thoughtful choices for your child and your community.
Questions to Ask If You Suspect Measles
If you think your child might have been exposed or is showing symptoms, ask yourself:
- Has your child been vaccinated? Even one MMR dose offers strong protection. Two doses mean even better, lasting immunity.
- Has your child traveled recently? International travel or trips to areas with outbreaks can increase risk.
- Has your child been exposed to anyone with measles? Consider schools, daycare, family events—measles is very contagious, even with brief contact.
- What symptoms are showing up?
- Is your child breathing comfortably? Watch for fast breathing, grunting, wheezing, or signs of distress. Seek immediate care if you see these.
These questions aren’t meant to add worry—they help you gather important details so you can get clear, effective guidance from your pediatrician or Poppins clinician.
When to Call the Pediatrician or Go to the ER
Measles isn’t always mild—and it can turn serious quickly in some kids. Don’t second-guess getting help if your child seems very sick. Trust your instincts, and know that your pediatrician or local emergency department is there to help you sort out what’s going on.
Red Flags for Immediate Medical Help
Call 911 or go to the nearest emergency department if you see any of these signs:
- Persistent high fever (≥104°F): Especially if it doesn’t come down with fever reducers or keeps coming back.
- Trouble breathing or rapid breathing: Any sign your child is struggling to catch their breath.
- Seizures: New or unexplained seizures always need urgent evaluation.
- Confusion or difficulty waking: If your child seems very drowsy, unresponsive, or isn’t acting like themselves.
- Worsening rash with bruising or petechiae: Small purple or red spots that don’t fade with pressure (aka petechiae) can signal bleeding under the skin and require immediate care.
“If you’re not sure, it’s always better to call,” says Kimmes. “We’d rather reassure you than have you miss something serious.”
Signs of Severe Illness in Kids
Call your pediatrician right away if you see these signs—they can get worse quickly in younger children:
- Dehydration: Look for fewer wet diapers or trips to the bathroom, dry mouth or lips, no tears when crying, or extreme thirst.
- Persistent vomiting: This can make dehydration worse and may signal a more severe infection.
- Lethargy or unusual fussiness: If your child is hard to comfort or seems unusually tired, it can be an early sign of complications.
Your pediatrician can help you decide whether you can continue supportive care at home or need to be seen right away.
Bottom line: When in doubt, call. It’s always okay to ask for help when your child is sick—especially with something as potentially serious as measles.
Diagnosing Measles in Children
If you suspect your child might have measles, getting a proper diagnosis is essential. Not only does it confirm what you’re dealing with, but it also helps protect others by preventing further spread. Your pediatrician is your best partner in figuring this out.
What Tests to Expect (Swabs, Bloodwork)
Diagnosis of measles relies on both your child’s symptoms and lab testing to confirm the virus and rule out other illnesses that can look similar. Here’s what might happen at the doctor’s office:
- Nasal or throat swabs: A small swab is used to collect secretions from the nose or throat to test for the measles virus itself.
- Urine tests: The virus can be detected in the urine, so your doctor may ask for a sample.
- Bloodwork: Blood tests can check for measles-specific antibodies that confirm infection.
These tests help your pediatrician be confident in the diagnosis and avoid unnecessary worry (or underestimating a real case).
Why Reporting to Public Health Matters
If your child is suspected or confirmed to have measles, your doctor is required to report the case to local public health authorities. This isn’t about getting anyone in trouble—it’s about protecting the community.
Here’s why it matters:
- Quick response: Health departments can track exposures and notify people at risk.
- Prevent outbreaks: Early identification limits spread, especially in schools or daycares.
- Protect vulnerable groups: Babies too young for vaccination, pregnant individuals, and immunocompromised people are at higher risk of severe illness.
Your doctor or Poppins clinician can explain how this process works and help you navigate any next steps with your local health department.
Measles Treatment in Kids
There’s no magic cure for measles—but there is a clear, evidence-based plan for caring for your child and keeping them as safe and comfortable as possible. The goal is to manage symptoms, watch for complications, and know when to escalate care.
No “Cure” for Measles—What Supportive Care Looks Like
Measles is caused by a virus, so antibiotics don’t work, and there’s no specific antiviral treatment. Instead, care is all about supporting your child while their immune system fights off the virus.
At home, this means:
- Fluids: Keeping your child well-hydrated is critical. Offer water, breast milk or formula for babies, electrolyte solutions, or diluted juice to help prevent dehydration—especially if they have fever or diarrhea.
- Fever control: Use age-appropriate doses of acetaminophen or ibuprofen to reduce fever and keep your child comfortable. Always follow dosing guidelines or your pediatrician’s advice.
- Rest and comfort: Make sure they get plenty of sleep and feel safe and soothed. Dim lights can help with light sensitivity caused by conjunctivitis.
- Close monitoring: Watch carefully for signs of breathing difficulty, confusion, dehydration (dry mouth, no urination, no tears), or other serious symptoms that need prompt medical care.
Role of Vitamin A (Use with Care)
Research has shown that Vitamin A supplements can reduce the risk of complications from measles in certain children, especially in areas where deficiency is common. It’s not a cure, but it can help the immune system respond better.
However, dosing matters: too much Vitamin A can be harmful since it’s fat-soluble and stored in the body. That’s why it should always be given under medical supervision. Your pediatrician or Poppins care team can advise you if Vitamin A is appropriate for your child’s case.
Exposure but No Symptoms? What Parents Should Do
Finding out your child was exposed to measles can feel overwhelming—especially if they aren’t sick yet. Here’s exactly what to do if you know or suspect they were exposed but don’t have symptoms (yet).
The goal is simple: prevent further spread and catch any illness early.
If Your Child is Fully Vaccinated: Monitor vs. Quarantine
The good news is that two doses of the MMR vaccine provide strong protection. Fully vaccinated kids can usually just be observed at home. Parents should watch carefully for symptoms (fever, cough, runny nose, red eyes, rash) over the 21 days after exposure. If any symptoms appear, keep them home, start quarantine immediately, and contact your pediatrician for next steps.
If Your Child Is Not Fully Vaccinated or Immunocompromised
Call your pediatrician right away. Post-exposure MMR vaccination may help if given quickly after exposure, and immune globulin (IVIG) may be recommended for certain high-risk children. In general, unimmunized children who have been exposed will need to quarantine for 21 days after the last known exposure—even if they seem completely healthy.
Importance of Family Immunizations
Even if your exposed child is healthy and vaccinated, make sure other family members are up to date on their MMR vaccines too. Vaccinating eligible family members helps create a protective circle around babies too young to get the shot, pregnant people, and immunocompromised loved ones who are especially vulnerable to severe measles complications.
Preventing Measles in Kids
Prevention is always easier (and less scary) than trying to manage an outbreak in your home or community. Here’s what you need to know to keep your child and others safe from measles.
The Importance of the MMR Vaccine
The MMR vaccine (measles, mumps, rubella) is the best defense against measles. In fact, ,easles was previously considered eliminated in the US in 2000, and has only come back because of a downtrend in immunizing. The vaccine is safe with very low side effects, highly effective, and part of the routine immunization schedule for kids in many countries.
Here’s what the typical MMR vaccine schedule looks like:
- First dose: Given at 12–15 months of age
- Second dose: Typically at 4–6 years
As discussed above, these two doses provide long-lasting immunity in most children and significantly reduce the risk of outbreaks in communities.
Measles was previously considered eliminated in the US in 2000, has only come back because of downtrend in immunizing
Keeping Your Family and Community Safe
It’s not just about shots—it’s also about the everyday choices that help reduce the spread of measles.
If your child is sick—even with early, mild symptoms like fever or cough—try these best practices to help protect others:
- Keep your child at home to avoid spreading illness.
- Encourage good hygiene, such as covering their mouth and nose when coughing or sneezing, washing hands frequently, and wearing masks if you need to visit healthcare settings where there’s concern for measles.
If there’s a known measles exposure in your community, stay alert for symptoms, follow local health department guidance, and don’t hesitate to reach out to your pediatrician or Poppins for advice.
Frequently Asked Questions from Parents
These are the top questions we hear from parents worried about measles. Let’s clear up confusion with simple, trustworthy answers you can actually use.
Is Measles Really That Serious in Kids?
Yes. Measles isn’t “just a rash”—it’s a highly contagious viral infection that can cause pneumonia, brain swelling (encephalitis), severe dehydration, and even death, especially in children under 5. That’s why vaccination is so important and why early detection matters so much.
For more detail, see What Is Measles (Rubeola) in Kids?
What Are The First Signs of Measles in Children?
The earliest signs usually include fever (often high), cough, runny nose (coryza), and red, watery eyes (conjunctivitis)—the classic “3 C’s.” These appear before the rash, making them the first clues for parents to watch for.
Learn more in Measles Symptoms in Children
How Does the Measles Rash Look?
The measles rash is deep red and blotchy. It typically starts on the face at the hairline, then spreads downward to the trunk, arms, legs, and feet. Small spots often merge into large patches, and the rash may leave a brownish discoloration as it heals.
See details in The Classic Measles Rash Explained
What Are Koplik Spots?
Koplik spots are small, bluish-white spots that appear inside the cheeks, often 1–2 days before the skin rash begins. They’re a classic sign that helps doctors confirm measles, but they can be easy for parents to miss.
Read more in Koplik Spots: The Tell-Tale Mouth Sign
When Is a Child With Measles Contagious?
Kids with measles are contagious for 4 days before the rash starts and 4 days after it appears—known as the “4 & 4 rule.” This means a child can spread measles even before you realize they’re sick.
Learn about timing in How Long Before Symptoms Appear?
When Should I Take My Child to The Doctor or ER For Measles?
Go to the doctor or ER immediately if your child has:
- Persistent high fever (≥104°F).
- Trouble breathing or rapid breathing.
- Seizures.
- Confusion or difficulty waking.
- Signs of dehydration (dry mouth, no urination, no tears).
- Worsening rash with bruising or petechiae.
It’s always better to call if you’re unsure.
Check When to Call the Pediatrician or Go to the ER for more guidance.
How Is Measles Diagnosed in Kids?
Doctors diagnose measles using a combination of your child’s symptoms and lab tests like nasal swabs, urine tests, or bloodwork. Suspected cases are reported to local health departments to help control outbreaks.
Find out more in Diagnosing Measles in Children
Is There a Cure For Measles?
There’s no antiviral cure for measles. Treatment is supportive: fluids to prevent dehydration, fever control, and monitoring for complications. Some kids need hospital care if the illness is severe. Vitamin A may help in certain cases but should be given under medical guidance.
See more in Measles Treatment in Kids
What If My Child Was Exposed But Has No Symptoms?
If your child is fully vaccinated, you can monitor them for symptoms over 21 days. If symptoms develop, quarantine immediately and call your pediatrician. If your child is not fully vaccinated or is immunocompromised, contact your doctor right away to discuss post-exposure options like MMR vaccination or immune globulin (IVIG).
See details in Exposure but No Symptoms? What Parents Should Do.
How Can I Prevent My Child From Getting Measles?
Vaccination is the best prevention. Make sure your child is up to date on the MMR vaccine. Avoid exposing others if your child is sick, and keep them home if there’s any risk they could spread the infection.
Read more in Preventing Measles in Kids.
How Poppins Can Help Your Family
You don’t have to navigate measles—or any childhood illness—alone. Poppins is here with trusted, around-the-clock pediatric support to help you keep your family safe and your worries in check.
24/7 Pediatric Guidance
- Anytime Access: Chat with experienced pediatric clinicians day or night—even when your child spikes a fever at 2 a.m.
- Real-Time Answers: Get clear, expert guidance for rashes, fevers, breathing concerns, and more, right when you need it.
- Reassurance You Can Trust: “Parents shouldn’t have to make these decisions in a vacuum,” says Kimmes. “We’re here to provide clear, calm guidance so you know your next best step.”
Personalized Action Plans
- Tailored Advice: No one-size-fits-all checklists. We’ll help you know exactly what to watch for and what to do next.
- Step-by-Step Plans: Includes when to isolate, monitor symptoms, or seek in-person care.
- Follow-Up Support: We check in so you’re never left wondering if you’re doing enough or too much.
Help Navigating Referrals
- Know When to Go: We’ll help you decide if and when in-person care is needed.
- How to Prepare: Learn how to call ahead to clinics or ERs, wear masks, and reduce exposure risks.
- Local Connections: We’ll help you find the right urgent care, hospital, or specialist—so you don’t feel lost in the system.
With Poppins, you’re never on your own. We’re here to help you spot it, stop it, and keep calm—even at 2 a.m. with a worried heart and a sick kid in your arms.
Final Thoughts
Measles is serious—but with awareness, vaccination, and a clear plan, you can protect your family and community. At Poppins, we’re here to help you spot it, stop it, and keep calm—even on the hardest parenting days.

