If there’s one phrase that strikes fear into the hearts of parents who let their kids run wild outside, it’s “I found a tick on them.” Ticks are tiny, sneaky, and creepy—but you don’t have to let them ruin your day (or your camping trip).
This guide breaks down exactly what to do if your child gets a tick bite, how to assess their risk for Lyme disease, when to call your doctor, and—best of all—how to prevent those little bloodsuckers from latching on in the first place. Because with the right know-how, you can go from panic to prepared in minutes.
Understanding Tick Bites in Children
Before you picture a horror movie of disease and drama, let’s get clear on what happens when a tick bites and why it matters for kids.
Ticks attach to the skin to feed on blood. While that’s gross enough, the real concern is that some ticks can transmit diseases—most notably Lyme disease. But not all ticks carry Lyme, and even those that do need to be attached for a certain length of time to transmit it.
“Ticks are common, especially in certain regions and seasons, but most bites are low risk if handled properly,” says Jessica Kimmes, pediatric nurse practitioner with Poppins. “Knowledge is your best defense.”
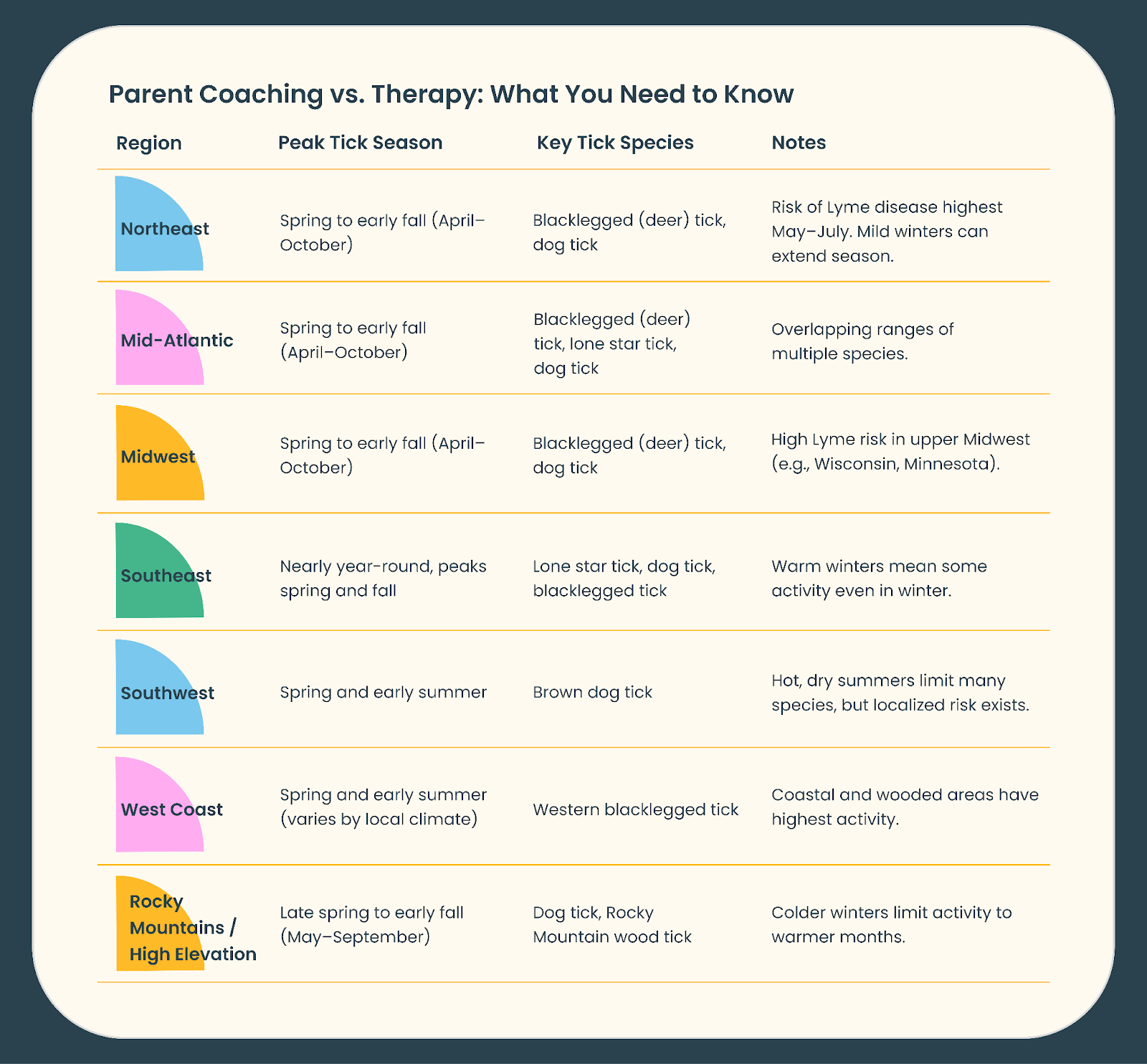
Here’s a summary of where and when ticks are most common:
Understanding the basics of tick bites can help you stay calm, take the right steps, and know when to watch for trouble.
What Happens When a Tick Bites?
Ticks use barbed mouthparts to anchor themselves into the skin. Once attached, they can stay for hours or even days if not removed.
“The longer a tick stays attached, the higher the risk of disease transmission,” Kimmes explains. “That’s why early removal is so important.”
While the bite itself is usually painless, the area can get red or irritated. This doesn’t automatically mean infection—it’s often just a local reaction.
Common Types of Ticks and How to Identify Them
Not all ticks are created equal when it comes to Lyme risk. These are the usual suspects you’ll see on kids (and pets) in tick-prone areas:
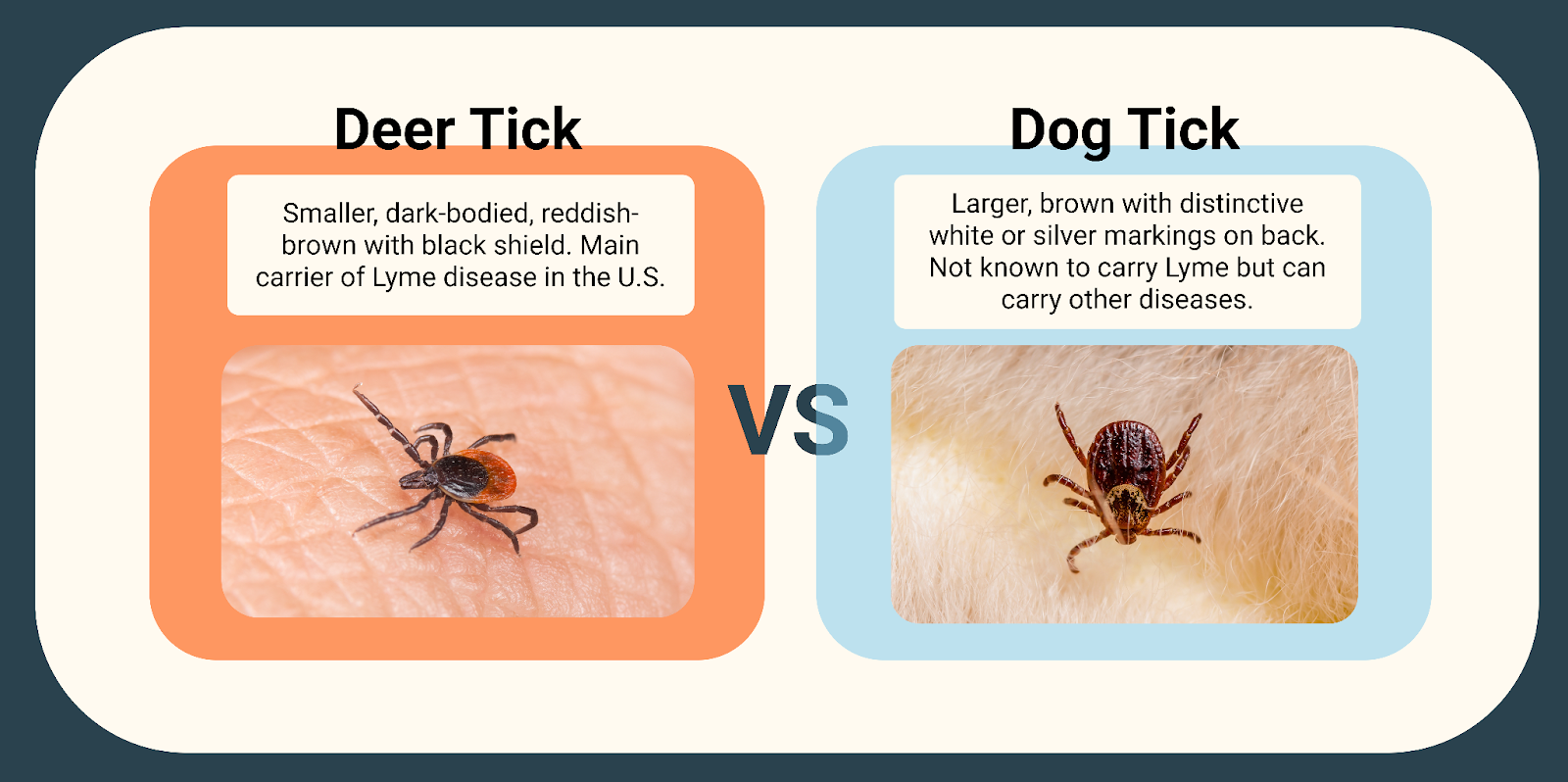
“Parents often can’t tell which tick it is,” Kimmes says. “If you can, take a picture or save the tick. It helps us assess risk.”
Knowing which tick bit your child (and how long it was attached) can help determine whether Lyme prophylaxis is needed.
Now that you know the players, let’s talk about what to do right after you spot a tick on your child.
Assessing a Tick Bite: What Parents Should Ask
You’ve found a tick on your child (or suspect you did). Breathe. The next step isn’t to panic—it’s to play detective. Careful assessment is how you figure out if there’s a real risk of Lyme disease or if you can just chalk it up as an outdoor nuisance. Here’s how to get the info you (and your pediatrician) will need to make that call.
Questions to Determine Risk
Start by asking these questions to figure out your child’s risk level and next steps:
- Was the tick seen or just suspected?
- Is it still attached?
- How long was it attached? Best guess is fine. The magic number? 36 hours. Deer ticks generally need to be attached at least 36 hours to transmit Lyme.
- Was the tick engorged (big and full of blood) or flat?
- Did you remove the entire tick, including the head?
- Did you save it or take a photo for ID?
Answering these questions will help you and your healthcare provider decide if further evaluation or treatment is needed.
Symptoms to Watch for After a Bite
Even if you removed the tick quickly, keep an eye out for these symptoms in the next days to weeks:
- Local redness or swelling at the bite site.
- A rash that looks like a bullseye (see picture below) or target lesion (classic sign of early Lyme).

“A local bump that’s red for a few days is normal,” says Kimmes. “It’s the expanding, target-like rash that’s concerning and what we want to monitor for.”
When to Worry About Lyme Disease
Lyme disease doesn’t appear instantly—it typically develops 3–30 days after a bite, and occurs in more than 70% of early Lyme disease cases.
“The hallmark is the erythema migrans rash,” Kimmes says. “It expands over days, often with a clear center. This is sometimes called a bullseye rash because it can look like a red ring with clearing in the middle. It’s not typically itchy or painful, but it slowly gets bigger over time. If you notice this kind of rash on your child, even if you didn’t see a tick, it’s important to talk with your healthcare provider.”
Call your pediatrician if:
- You see a spreading bullseye rash.
- Your child develops fever, headache, joint pain, or facial droop.
- Symptoms appear weeks or months after the bite, like joint swelling or neurological changes. Notably, these symptoms can appear without a known tick bite or bullseye rash.
If you suspect Lyme Disease in your child, here is a detailed breakdown of the different stages.
Stages of Lyme Disease in Kids
Lyme disease isn’t a single, uniform illness—it develops in stages, and the symptoms can look very different depending on how long it’s been since the tick bite. Knowing these stages helps you recognize early warning signs (when treatment is easiest) and understand when it’s time to escalate care. Let’s break it down so you know exactly what to watch for.
Early Localized Lyme Disease
This is the stage most parents have heard about—and the one you really want to catch early. Early localized Lyme disease typically develops 3–30 days after a tick bite, when the bacteria is still close to the site of entry. Recognizing this stage is important because treatment is most effective here.
Here are the key features of early localized Lyme Disease to be on the lookout for:
- An expanding red rash (erythema migrans) that may look like a warm, target-shaped “bullseye,” often painless or mildly itchy. The Rash can appear at the bite site or elsewhere on the body.
- Mild systemic symptoms such as fever, fatigue, headache, or muscle aches.
Prompt antibiotic treatment at this stage is highly effective and can prevent progression to later stages.
Early Disseminated Lyme Disease
If untreated, Lyme can spread through the bloodstream to other parts of the body over weeks to months.
Symptoms may include:
- Multiple erythema migrans lesions in different locations.
- Fever, chills, fatigue.
- Headache, stiff neck.
- Migratory joint pain (comes and goes in different joints).
- Facial nerve palsy (sudden drooping on one side of the face).
- Heart involvement (rare in kids but can cause rhythm changes).
“Facial droop is one of the classic signs of early disseminated Lyme in kids,” Kimmes explains. “If you see it, call your pediatrician right away—it needs evaluation.”
This stage requires prompt medical assessment and often a longer course of antibiotics.
Late Lyme Disease
This stage can occur months to years after an untreated infection.
Key features of late Lyme Disease include:
- Persistent or intermittent joint swelling, especially large joints like the knees.
- Chronic arthritis-like symptoms.
- Rare neurological issues (numbness, tingling, memory problems).
“Late Lyme is less common thanks to good awareness,” Kimmes says. “But it’s a big reason we push early recognition and treatment—it’s preventable.”
Late Lyme disease can be serious but is still treatable with antibiotics, though symptoms may take longer to resolve. Recognizing these stages—and knowing when to act—makes a huge difference. If you’re ever unsure about a rash, new joint pain, or weird neurological symptoms in your child after a tick bite, don’t guess. Call your pediatrician or reach out to Poppins. We’re here to help you navigate every stage with confidence.
How to Remove a Tick Safely
Tick removal doesn’t have to be a battle—promise. This part is all about clear, practical steps that actually work (and avoiding the old wives’ tales that can make things worse). If you’ve spotted a tick on your child, here’s exactly how to get it off quickly and safely.
Step-by-Step Tick Removal Guide
Here’s the safe, recommended way to remove a tick without making things worse:
- Use fine-tipped tweezers.
- Grasp the tick as close to the skin’s surface as possible.
- Pull upward with steady, even pressure. Don’t twist or jerk.
- If mouth-parts remain, try removing them with tweezers. If they’re stuck, leave them alone to let the skin heal.
- Clean the bite area and your hands with soap and water or rubbing alcohol.
- Dispose of the tick by sealing it in a bag, submerging in alcohol, or flushing it.
“If you can, take a photo of the tick,” Kimmes suggests. “It helps us confirm it’s a tick and ID what type later.”
What Not to Do When Removing a Tick
Skip these old-school methods—they don’t work and can increase the risk of problems:
- Petroleum jelly. Smearing thick jelly over the tick in hopes of suffocating it.
- Nail polish. Painting over the tick to try to seal it off and make it back out.
- Isopropyl alcohol to suffocate the tick. Pouring or dabbing alcohol directly onto the tick to kill it while attached.
- Burning with a match. Touching a hot match or heated object to the tick to force it to detach.
These “tricks” might sound clever, but they don’t actually make the tick let go safely. Instead, they stress or injure the tick while it’s still embedded, making it more likely to regurgitate saliva or gut contents into the bite. That can increase the chance of transmitting infections like Lyme disease.
The safest approach is to use fine-tipped tweezers to grasp the tick close to the skin and pull it out steadily and gently.
Cleaning and Disposing of the Tick
After removal, clean the area well. Store the tick if your pediatrician recommends. Otherwise, kill it in alcohol or flush it.
Treatment and When to Seek Care
Not every tick bite needs a prescription or a panicked drive to urgent care. But you do want to know what to watch for and when to act. Let’s break down what counts as a normal reaction, what might mean infection, and when your child might need antibiotics to prevent Lyme disease.
Local Reactions vs. Infection
A small red bump at the bite site is normal. This is your child’s skin reacting to the tick’s bite—just like it would to a mosquito or insect bite. It might be a bit itchy or slightly swollen, but this doesn’t mean Lyme disease—it’s just local irritation.
Here’s when to be concerned about infection:
- Redness that keeps spreading significantly outward.
- Area becomes warm to the touch.
- Pus or drainage from the bite.
- Increasing pain at the site.
- Fever developing a few days after the bite.
These are signs of a bacterial skin infection (cellulitis), which can happen when bacteria on the skin enter the tiny wound left by the tick bite. If you see signs of infection, your child may need antibiotics.
“Treat a local infection like any other cellulitis,” Kimmes says. “That’s separate from Lyme risk.”
When Lyme Prophylaxis Is Recommended
Prophylactic antibiotics aren’t needed for every tick bite. They're recommended only if all of these apply:
- The tick is identified as a deer tick in a high-risk area (local Lyme prevalence ≥20%).
- Estimated attachment time is 36 hours or more.
- The dose can be given within 72 hours of tick removal.
If these criteria are met, your pediatrician may recommend giving your child a one-time dose of doxycycline (adjusted for their weight) to help prevent Lyme disease. This antibiotic is generally safe but isn’t right for every child—for example, it may not be recommended for very young children or for those with certain medical conditions like myasthenia gravis or who are taking medications such as Accutane. Your doctor will help decide if it’s the best option for your child.
Lyme Disease Treatment and Referral
If your child develops erythema migrans (the classic bullseye rash), fever, or other Lyme disease symptoms, it’s important to act quickly:
- Call your pediatrician for guidance.
- Blood testing may be recommended in some cases.
- Antibiotic treatment typically lasts 10–21 days and is tailored to your child’s age and specific symptoms.
“Early treatment is effective and prevents complications,” Kimmes reassures.
For signs of more advanced Lyme disease—like joint swelling, facial weakness (palsy), or neurologic symptoms—your child will need an in-person evaluation and may require referral to a specialist for further care.
Of course, the best treatment is prevention. Next, let’s talk about how to keep those ticks off your kids in the first place.
Prevention: How to Protect Your Child from Ticks
Look, you don’t have to keep your kid indoors forever to avoid tick bites (unless you want to lose your mind). Prevention is about smart, doable habits that reduce the chance of ticks latching on in the first place. Here’s how to keep those bloodsuckers off your child without killing their love of the outdoors.
Best Practices for Avoiding Tick Bites
These simple steps can go a long way toward keeping ticks off your child:
- Stay on clear trails when hiking.
- Avoid tall grass and dense brush.
- Wear light-colored clothing to spot ticks more easily.
- Tuck pants into socks or boots.
“These little steps make ticks easier to spot and stop,” Kimmes says.
Recommended Tick Repellents and Clothing
Here are parent-approved repellents and clothing tips that actually work:
- Use EPA-registered repellents with 20–30% DEET (safe over 2 months old), picaridin, or oil of lemon eucalyptus (not for kids under 3).
- Treat clothing with an insecticide like permethrin (never on skin).
“Repellents are safe when used as directed,” Kimmes reassures. “They’re one of our best tools.”
Performing a Full-Body Tick Check
A good tick check can catch even the sneakiest hitchhikers—here’s how to do it:
- Check kids within 2 hours of coming indoors.
- Focus on: scalp, behind ears, underarms, waistline, groin, behind knees.
- Shower within 2 hours of exposure.
- Put clothes in a hot dryer for 10 minutes to kill ticks.
And if you’re struggling to keep your little one still for the check, here are some tips to make it easier (and even a little fun):
- Turn it into a “tick inspection game” with a silly flashlight or magnifying glass.
- Make up a “tick-check song” you sing while looking.
- Let them “help” inspect a parent or sibling first.
- Do the check while reading a bedtime story or watching a favorite show to keep them still.
- Offer a small reward or sticker for being patient.
“I tell families: make tick checks part of the post-adventure routine,” Kimmes says.
Parent FAQs: Tick Bites and Lyme Disease
Parents have a lot of questions about ticks—and for good reason. They’re small, sneaky, and come with plenty of scary headlines. Let’s cut through the panic with clear, practical answers you can actually use when your kid comes running in from the backyard saying, “I think there’s something on me!”
How Long Does a Tick Need To Be Attached To Transmit Lyme?
Ticks don’t transmit Lyme immediately. In most cases, the deer tick (Ixodes scapularis) needs to be attached for at least 36 hours to transmit the bacteria that causes Lyme disease.
“This is why prompt removal matters so much,” says Kimmes. “If you catch it early, you dramatically reduce the risk.”
If you’re not sure how long the tick was attached, think back: when was the last time you know that body area was clear? That can help your provider assess risk.
What Does a Lyme Disease Rash Look Like?
Lyme’s most famous sign is the erythema migrans rash—a red, expanding lesion with central clearing that creates a “bullseye” or “target” pattern.
But heads-up:
- It doesn’t always look perfect. It can be solid red or oval.
- It usually appears 3–30 days after the bite.
- It expands over days, not hours.
Always take a photo if you see an expanding rash—it helps your pediatrician make the call.
Should I Save The Tick for Testing?
Here’s the deal: tick testing isn’t recommended for determining Lyme risk. Even if the tick tests positive, it doesn’t mean your child was infected.
Instead, take a photo of the tick so that your provider can confirm the species (deer tick vs. dog tick). Then make sure you dispose of the tick properly by flushing it or sealing it in a bag (so it can’t get out) and throwing it in the trash.
Can My Child Get Lyme Disease More Than Once?
Yes. Unfortunately, Lyme disease doesn’t provide lifelong immunity. Kids can get it again with future bites from infected deer ticks. That’s why prevention remains so important, even after a past infection.
“We see repeated Lyme cases in high-risk areas,” Kimmes notes. “It’s all about staying vigilant every season.”
Are All Ticks Dangerous?
No. Deer ticks (Ixodes) are the main concern for Lyme disease in the U.S. and even then, not every deer tick is infected with Lyme-causing bacteria. Dog ticks and lone star ticks don’t typically transmit Lyme but can carry other diseases.
What If Part of The Tick Is Still in The Skin?
If the tick’s mouth-parts break off and stay in the skin, don’t panic.
- Try to remove them with clean tweezers if possible.
- If you can’t, leave them alone. The skin will usually push them out naturally over days.
“Digging too aggressively can cause more harm than good,” Kimmes warns. Keep the area clean and watch for signs of local infection like redness that spreads, pus, or pain after a couple of days.
Should My Child Take Antibiotics Just in Case?
Great question. The answer is not automatically. Prophylactic antibiotics (a single dose of doxycycline) are only recommended if:
- The tick is identified as a deer tick in a high-risk area.
- It was attached for 36 hours or more.
- The dose can be given within 72 hours of removal.
“We want to avoid unnecessary antibiotics,” Kimmes explains. “But in the right situation, they’re absolutely the right call.” Your pediatrician will help you decide if prophylaxis is warranted.
How Can I Reduce the Risk of Tick Bites in The First Place?
Prevention is your best defense.
- Use EPA-registered insect repellents (DEET, picaridin).
- Dress kids in long sleeves and pants.
- Treat clothing with permethrin.
- Do thorough tick checks after outdoor play.
- Shower within 2 hours of being outdoors.
- Dry clothes on high heat for 10 minutes.
Wrapping It Up: Handling Ticks Like a Pro (and Knowing When to Call Us)
Ticks are creepy—but you don’t have to be unprepared. By learning how to prevent bites, remove ticks safely, recognize early Lyme symptoms, and know when to seek care, you can keep your kid safe without losing your sanity.
And if you ever need help—whether you’re staring at a tick you just pulled out or worrying about a rash days later—Poppins is here for you. Sign up today and get 24/7 access to expert pediatric guidance, so you’re never left guessing when it matters most.

