Fast Facts About Dehydration in Kids:
- 75% of hospitalized dehydration cases are from vomiting/diarrhea
- Toddlers need ~4–8 cups of fluids daily
- Popsicles count toward hydration!
If your child is suddenly cranky, clammy, or unusually quiet, dehydration might be stealing their spark. And while thirst alone isn't an emergency, dehydration can turn dangerous fast—especially in young children. Let’s break it down: what’s normal, what’s not, and what to do when your child’s fluid tank starts running low.
In this guide, we’ll walk through the signs of dehydration in a child, when to worry, and how to rehydrate fast (even when your kid won’t touch Pedialyte with a ten-foot straw). We’ve also included expert insight from Poppins pediatric nurse practitioner Lisa Braunwell and real-world rehydration tips to get your little one back to baseline.
Two Main Causes of Dehydration in Kids
Let’s talk about the usual suspects behind a child’s dehydration. There are two most common causes:
1. Gastrointestinal Illness (a.k.a. the barf-and-poop parade)
Whether it’s a stomach virus, food poisoning, or something they picked up at daycare, vomiting and diarrhea are top causes of fluid loss in kids.
2. Heat Exposure or Excessive Activity
Summer sports, long days at the beach, or even just skipping water during hot weather can all lead to heat-related dehydration.
Other contributors include high fevers, certain medications, and even chronic conditions like diabetes.
What Are the Key Signs of Dehydration in a Child?
Kids can go from bouncing off the walls to running on empty faster than you’d expect. That’s why it’s so important to catch dehydration early—before it spirals into something more serious.
Here are 10 signs of dehydration in kids to watch for:
- Less active or playful than usual
- Fewer wet diapers (infants should have at least 6 per day)
- Toddler dehydration face signs (dry mouth or cracked lips)
- Fewer or no tears when crying
- Fussiness or irritability
- Headache or complaints of dizziness
- Weakness or low energy
- Nausea or vomiting
- Muscle cramps
- Cool or mottled hands and feet (aka patchy or blotchy, with irregular areas of pale and reddish-purple coloring)
Expert-Backed Ways to Treat Mild Dehydration at Home
So your kid’s running low on fluids—but not showing signs of serious distress. Now what?
Here’s what is the fastest way to hydrate a child (and how to actually get them to drink something):
General Tips for Rehydration:
- Offer small, frequent sips rather than large gulps. Small sips are easier for the stomach to tolerate—especially if your child is nauseous or has been vomiting. Gulping too much at once can trigger more vomiting or stomach cramps, making dehydration worse.
- Use oral rehydration solutions like Pedialyte or Gatorade (depending on age). These fluids are specially formulated with the right balance of electrolytes (like sodium and potassium) and sugar to help the body absorb water more efficiently. For young kids and infants, Pedialyte is gentler and safer than sports drinks, which can contain too much sugar.
- Stick to water for older kids without vomiting or diarrhea. If your child isn’t losing a lot of electrolytes through vomiting or diarrhea, plain water is usually all they need to stay hydrated. It replenishes fluids without adding unnecessary sugar or additives.
- Avoid sugary drinks and fruit juices—they can worsen diarrhea. High-sugar drinks can pull more water into the intestines, which can actually make diarrhea worse. They also lack the precise electrolyte balance needed for effective rehydration.
- Encourage rest in a cool, shaded area. Activity and heat can cause kids to lose even more fluids through sweat. Cooling down reduces fluid loss and gives the body a better chance to recover and absorb the fluids they’re taking in.
If Vomiting Is Involved:
- Wait 30–60 minutes after vomiting before reintroducing fluids. Giving the stomach a short break allows it to settle and reduces the chance of triggering another vomiting episode. Jumping in too quickly can restart the cycle and make it harder to keep fluids down.
- Start with 1–2 teaspoons (5–10 mL) every 5 minutes for infants. Tiny, measured amounts are much easier for sensitive stomachs to tolerate. This slow-drip approach helps the body absorb fluids without overwhelming the digestive system.
- Gradually increase volume as tolerated. Once your child keeps down small sips, gradually increasing the amount allows the body to rehydrate more effectively without risking a setback (like vomiting again).
- For breastfed babies: nurse in short, frequent intervals. Short feeds are easier to manage if a baby is queasy, and frequent nursing keeps them hydrated while minimizing the risk of vomiting. It also maintains comfort and bonding during illness.
- Spoon or syringe-feeding may help with younger babies. When a baby refuses to latch or struggles with a bottle due to nausea, spoon or syringe feeding allows for more control. You can deliver tiny amounts slowly, which makes it easier for them to tolerate.
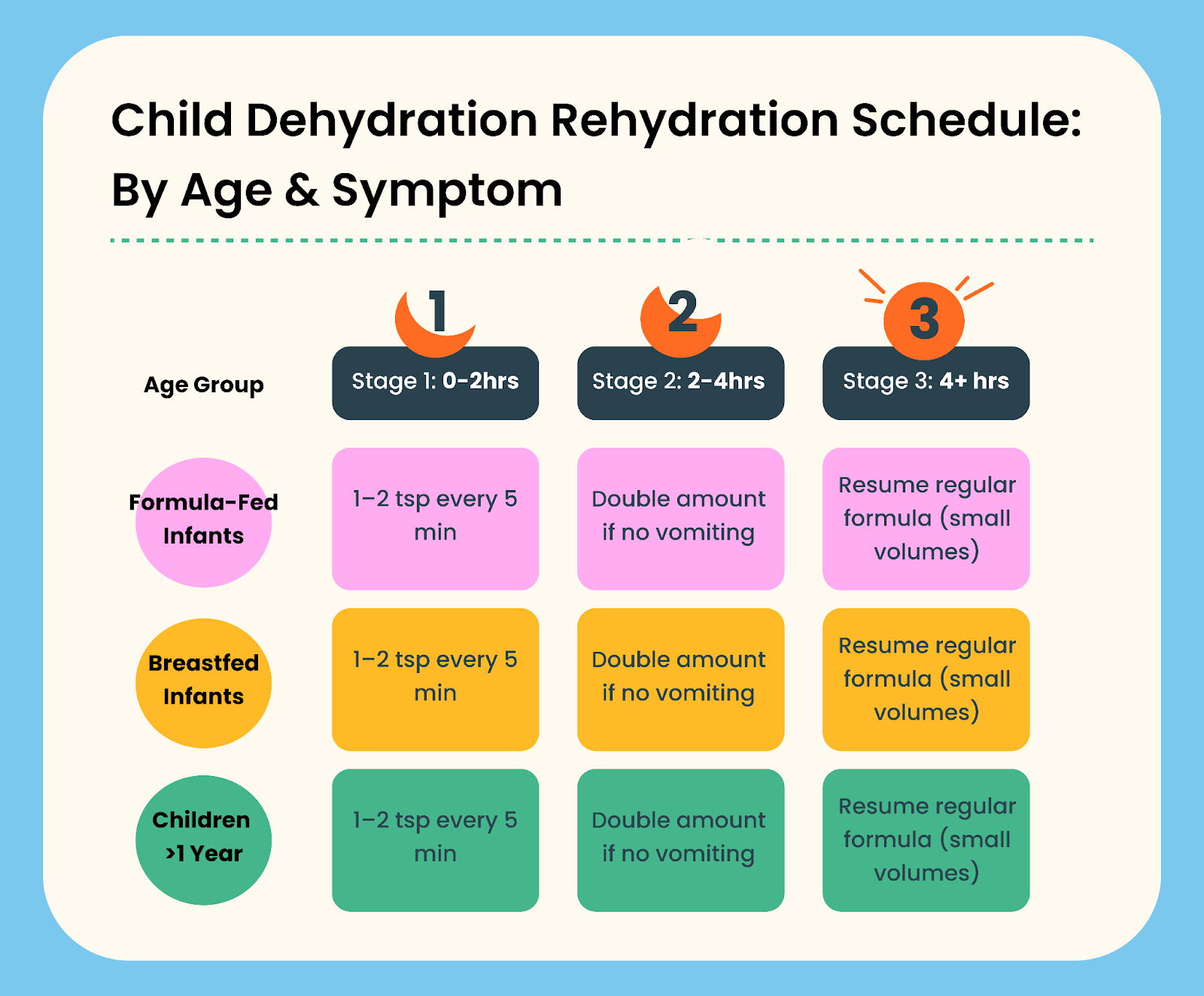
Comprehensive Rehydration Schedule for Different Ages
Here’s a quick-reference guide to keep hydration on track, even when your child isn’t thrilled about drinking anything:
How To Manage Rehydration Battles
Alright, parents—let’s get real. Hydrating a sick kid can feel like trying to water a cactus that bites back. They’re nauseous. They’re grumpy. They hate Pedialyte with the fire of a thousand suns.
Here’s how to play the hydration game like a pro:
- Make it fun: Offer fluids in a silly cup, through a straw, or with a popsicle twist. If your toddler wants to sip from your smoothie tumbler like a tiny influencer? Let them.
- Don’t bribe, narrate: “Ooh, you took a sip! That’s one sip closer to your superhero powers coming back.” Enthusiasm is contagious.
- Keep it visible: Put a cup within arm’s reach—no chasing required.
- Offer choices: “Do you want blue drink or orange? Straw or no straw?” Let them feel in control.
And if none of it works? Text your Poppins provider. We’re here as backup when you need it.
Signs of Severe Dehydration: When to Seek Emergency Care
Most cases of dehydration can be managed at home. But there are certain red flags that signal it’s time to seek immediate medical care.
If you’re wondering, When should I take my child to the ER for dehydration?—here’s your checklist:
- Urinating only once or twice a day (or not at all)
- Extreme lethargy or difficulty waking
- Inability to keep down any fluids
- Sunken soft spot (fontanelle) in infants
- No tears when crying
- Bloody vomit or diarrhea
- High fever with other concerning symptoms
- Severe abdominal pain
- Bile-colored (green/yellow) vomit
These are considered danger signs of dehydration and should prompt a call to your pediatric provider or a visit to the ER.
What About IV Fluids?
Many parents ask: How do I know if my child needs IV fluids for dehydration?
IV fluids are typically reserved for children who:
- Cannot keep any fluids down
- Show signs of moderate to severe dehydration
- Are lethargic, weak, or inconsolable
- Have lost significant weight from illness
Lisa Braunwell adds: “In most cases, we can avoid the ER with early and consistent oral rehydration. But if we’re seeing red flags or your child isn’t bouncing back, we’ll help you make that call.”
Dehydration in Babies: Why It Can Be Riskier
Babies are tiny humans with tiny fluid reserves—so even mild dehydration can hit hard and fast.
Since they can’t tell us how they’re feeling, here’s what to look for:
- Fewer than 6 wet diapers in 24 hours
- Dry lips and mouth
- Trouble latching or feeding
- Limpness or floppiness
- Less alert or responsive
- Sunken fontanelle (soft spot on the head)
Timeliness is key. As Lisa explains, “with babies, the window to act is shorter. If your infant is refusing feeds or seems more sleepy than usual, it’s best to check in with a provider quickly.”
Chronic Dehydration Symptoms: What to Watch for Long-Term
While most dehydration is short-term, some kids—especially picky eaters or those with sensory sensitivities—may not drink enough regularly.
Possible signs of chronic dehydration in children:
- Frequent headaches
- Constipation
- Dry skin or lips
- Low energy or fatigue
- Trouble concentrating
- Dark yellow urine
If this sounds like your child, talk to your pediatric provider or Poppins pediatric care team about ways to build hydration habits into your daily routine.
Dehydration Prevention Tips for Parents
You can’t force water down a toddler’s throat (and you shouldn’t). But you can set the stage for good hydration.
Here’s how:
- Encourage sips of water throughout the day—not just at meals
- Pack water bottles for car rides, playground visits, and outings
- Set reminders to hydrate during outdoor activities
- Add fun: silly straws, colored ice cubes, or frozen fruit in water
- Keep sports drinks or Pedialyte on hand for illness or heat exposure
- Choose hydration foods for picky eaters: watermelon, cucumber, yogurt
Pro Tip: During hot weather, make sure kids hydrate before, during, and after outdoor play—even if they say they’re “not thirsty.”
Looking for a visual aid? This simple checklist helps you stay one step ahead, so your kid stays cool and energized this summer.
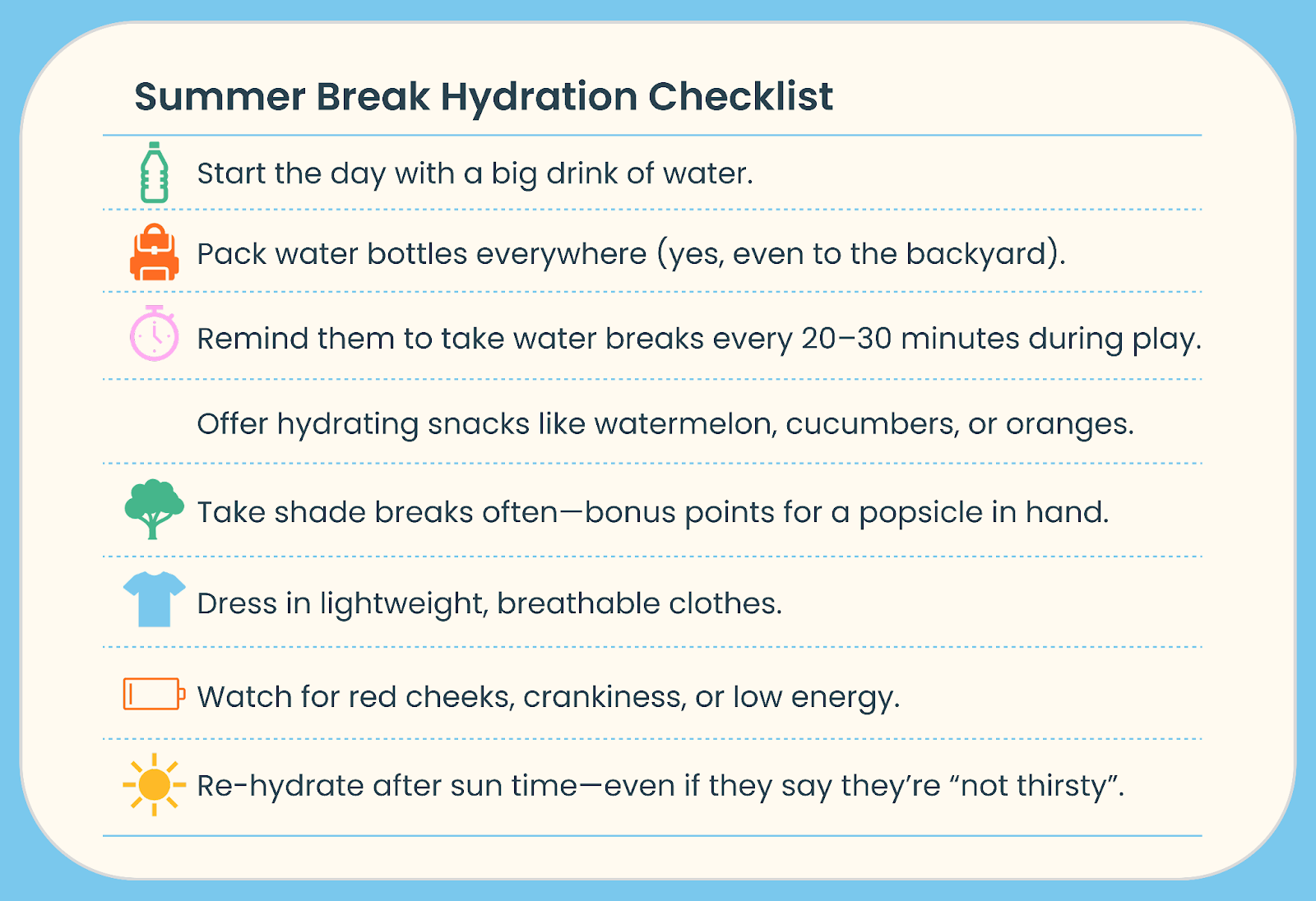
Hydration doesn’t have to be a power struggle. With a little planning (and maybe a popsicle bribe), you can keep summer fun flowing—without letting dehydration crash the party.
Parent FAQs: Dehydration Concerns Answered
Q: Can teething cause dehydration?
A: Yes. Excessive drooling during teething may lead to fluid loss, and some babies drink less due to gum pain. Monitor wet diapers—if fewer than 6 per day (or unusually dark urine), offer small sips of water (if over 6 months) or increase breastfeeding/formula.
Q: Does breastfeeding protect against dehydration?
A: Yes, breastmilk provides hydration and electrolytes. However, if your baby shows signs like fewer wet diapers, sunken soft spots, or lethargy, contact your provider—even breastfed babies can become dehydrated during illness or heat exposure.
Q: How to check a baby’s fontanelle for dehydration?
A: Gently feel the soft spot on their head when calm. A sunken fontanelle (dips inward) signals dehydration and requires immediate medical attention, especially with other red flags like no tears or extreme sleepiness.
When to Follow Up After a Dehydration Episode
At Poppins, we don’t just hand you a plan and ghost you. Our care team follows up to make sure your child’s symptoms are improving and you’re not navigating recovery alone.
After your visit, you’ll receive:
- A written action plan with clear hydration steps
- A follow-up message 24 hours later to check in
- Specific guidance on what symptoms mean it’s time to re-evaluate
This isn’t your average “wait and see” advice. It’s smart, proactive care—with pediatric experts by your side, even at 2 AM.
Final Thoughts: Trust Your Gut (and Your Poppins Team)
Dehydration is common—and it’s treatable. The key is catching it early, hydrating smart, and getting help when you need it.
Still not sure if your kid is dehydrated? That’s why we’re here. Whether it’s a mild case or something more serious, Poppins connects you with pediatric experts who can assess, guide, and follow up—all from your phone.
Because sometimes, knowing you’re not in this alone is the most powerful remedy of all.

