Coughs are the soundtrack of childhood. One kid brings home a bug from daycare, and suddenly it feels like your entire winter is scored by hacking fits and midnight wake-ups. But what happens when that cough just doesn’t go away?
If your child’s cough has lasted weeks instead of days, you’re probably wondering: Is this normal? Is it allergies? Asthma? Something worse? Do they need antibiotics?
This guide is your no-nonsense roadmap for understanding chronic cough in kids, figuring out when to worry (and when not to), and knowing how to help your child breathe easier.
Understanding Chronic Cough in Children
Before you panic over every cough that lingers, let’s talk about what “chronic” actually means.
A cough is one of the most common symptoms that brings families to the pediatrician. It’s also one of the trickiest to pin down, because so many conditions can cause it—and some kids seem to cough for weeks after every cold.
But here’s the first key: not all lingering coughs are a problem.
Jackie Jimenez, Family Nurse Practitioner at Poppins, explains: “Parents understandably get anxious about a cough that won’t quit. But many post-viral coughs can last three or four weeks and still be normal. The real question is: what other symptoms are there, and how is the child acting overall?”
Knowing what’s normal—and what’s not—can save you worry, unnecessary doctor trips, and a lot of lost sleep.
What Counts as a Chronic Cough?
Doctors usually call a cough chronic when it lasts more than four weeks. That’s because even an uncomplicated cold or viral infection often leaves behind an irritated, inflamed airway that takes time to calm down. Think of it like a scraped knee that’s still tender long after the scab forms.
But once you pass the four-week mark, it’s time to ask: is there an underlying cause that needs specific treatment? “Four weeks is our rule of thumb,” Jackie says. “Past that, we want to think about things like asthma, allergies, reflux, or even infection that needs antibiotics.” Before you stress, around 20% of coughing in young children lasts beyond the four-week mark, and around 5-10% of kids in the U.S. are affected by it. Chronic cough is not a rare condition, though it does warrant attention.
Common Causes of Persistent Cough
The good news? Most chronic coughs in kids have straightforward, treatable causes once you figure out what’s going on.
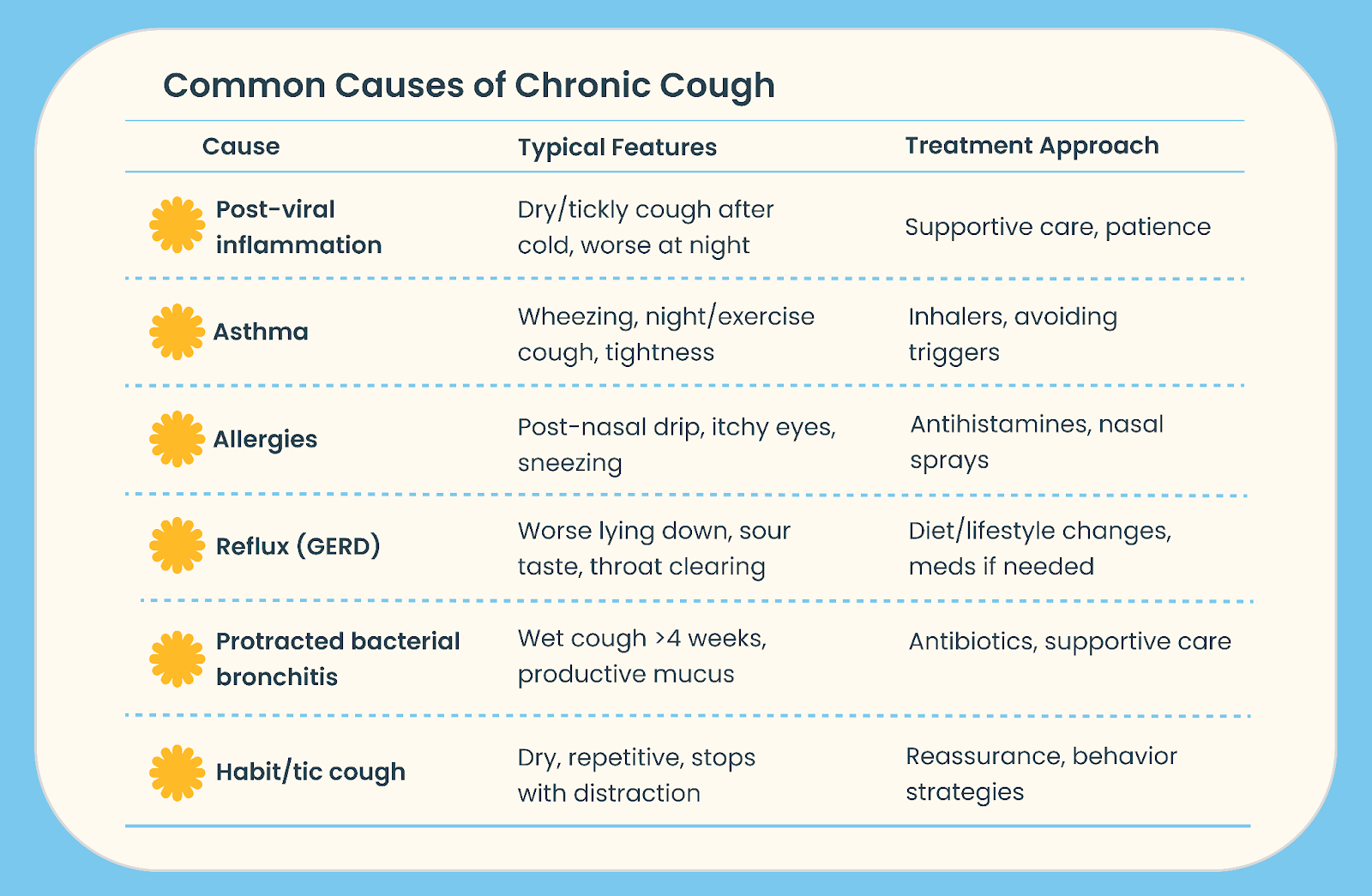
The below table summarizes the most common causes of chronic cough in children:
“Cough is a symptom, not a diagnosis,” Jackie explains. “Our job is to figure out the ‘why’ so we can treat it effectively.”
Recognizing Symptoms That Matter
When your kid’s been coughing for weeks, it’s easy to feel like you’re losing your mind—and your judgment. Is it just a cold? Do they need antibiotics? Urgent care? This is where knowing which symptoms matter helps you avoid both unnecessary panic and dangerous delays.
Typical Symptoms of a Lingering Cough in Children
First, let’s talk about what’s normal-ish. Typical lingering cough after a viral infection can be:
- Dry or tickly, especially at night.
- Worse with activity, dry air, or talking a lot.
- Mildly annoying but not interfering with sleep or play much.
When the above symptoms are present, it often just requires supportive care and patience.
Concerning Symptoms to Watch For
Not all coughs are created equal. Watch for these signs that mean it’s time to check in with your pediatrician:
- Wet cough lasting over 4 weeks. This may signal bacterial infection or underlying lung issues.
- Wheezing or whistling sounds. Suggests airway narrowing, classic for asthma.
- Cough waking child every night. Can indicate asthma or uncontrolled allergies.
- Weight loss, fatigue, poor appetite. Signals the cough is affecting overall health.
- Cough after choking. Raises concern for something lodged in the airway.
- Coughing up blood. Even small streaks need evaluation.
- Barking or whooping sounds. Think croup or pertussis, both need medical care.
- Night sweats or recent travel to TB areas. Red flags for tuberculosis.
Jackie says: “I don’t want parents to panic over every cough, but these symptoms are our cues to take it seriously and make sure we’re not missing something bigger.”
Red Flag Signs That Need Urgent Care
There are times you don’t want to wait for the pediatrician. If your child has any of these, it’s an urgent care or ER situation:
- Labored or fast breathing.
- Cyanosis (blue lips or face).
- Stridor (harsh, high-pitched noise when inhaling).
- Severe lethargy or confusion.
- Seizures.
- Persistent vomiting with dehydration signs.
Jackie explains: “Breathing trouble is a no-brainer. But don’t ignore mental status changes—being unusually sleepy or confused is a big red flag.”
Assessment Questions for Parents
When you do see your pediatrician, you can help them enormously by being ready to answer a few key questions. These details don’t just sound thorough—they actually shape the entire differential diagnosis and guide next steps.
How to Describe Your Child’s Cough
One of the biggest ways you can help your pediatrician is by giving a clear, detailed description of what you’re actually hearing. Vague words like “bad” or “constant” won’t tell the clinician much about the cough. But don’t worry—you don’t need a medical degree to do this well.
Here are some descriptors that can help:
- Is it wet or dry?
- Productive (bringing stuff up) or non-productive?
- When is it worst? (after meals, at night, outside)
- Any triggers? (exercise, allergens)
- Does it improve with distraction or worsen with stress? (habit/tic cough clue)
Key Details to Share with Your Pediatrician
So you’ve started listening to how your child coughs—awesome. Now let’s talk about the context around the cough.
It’s helpful to think about:
- When did it start? How long has it been going on?
- Has it improved, worsened, or stayed the same?
- Past history of asthma, allergies, reflux.
- Recent illnesses or back-to-back infections (common in daycare/school kids).
- Any choking episodes (foreign body risk).
- Recent travel or TB exposure.
- Impact on sleep, eating, play.
When to See the Doctor About a Persistent Cough
Here’s the million-dollar question: When do I actually make an appointment?
Let’s clear that up, once and for all. “Not every cough needs a visit today,” says Jackie Jimenez, Family Nurse Practitioner at Poppins. “But there are clear times when we want to see your child in person.”
How Long Is Too Long?
The first rule of thumb for coughs is: If the cough has lasted more than four weeks, see your pediatrician. Four weeks is the cutoff for chronic cough in children, but studies have shown over 60% of children to be still coughing after two months. Anything shorter is usually post-viral and may just need supportive care. But beyond that, we start thinking about underlying causes that need targeted treatment.
That said, duration isn’t everything. Even before four weeks, see your pediatrician if the cough is:
- Consistently wet and producing phlegm.
- Accompanied by wheezing or breathing difficulty.
- Waking them up frequently at night.
- Leading to weight loss, fatigue, or poor appetite.
- Happening after a known choking episode.
When to Head to the ER or Urgent Care
Okay—so much of this guide is about watchful waiting and knowing when to call your pediatrician. But let’s be clear: there are moments when you don’t wait at all.
These are the symptoms that mean your child needs to head straight to the ER:
- Trouble breathing or fast, labored breathing.
- Blue lips or face (cyanosis).
- A harsh, high-pitched noise when breathing in (stridor).
- Confusion, severe lethargy, or difficulty waking up.
- Seizures.
- Persistent vomiting with dehydration (fewer wet diapers, no tears, dry mouth).
These are all signs of serious illness that need immediate care. Jackie says: “Your instinct matters. If your gut says they’re struggling, don’t wait—get them seen right away.”
Treatment Options for Chronic Cough in Kids
So what happens once you see your pediatrician? The good news is, most causes of chronic cough in kids are treatable once you figure out the root cause. Let’s break down the common culprits—and what actually helps.
Managing Post-Viral Cough
Post-viral cough happens because the airways stay inflamed and sensitive long after the infection clears. It doesn’t mean the virus is still active, and it doesn’t mean your child needs antibiotics.
Here are some at-home care tips to that when combined with patience, can comfort your child while their body continues healing:
- Cool mist humidifier to soothe dry airways.
- Saline nasal spray to clear congestion.
- Warm fluids like tea or broth to ease throat irritation.
- Honey (for kids over one year old) to calm the cough reflex.
- Staying hydrated to keep mucus thin.
And yes—it’s usually fine to send them to school or daycare if they’re otherwise feeling okay.
Treating Asthma-Related Cough
Asthma is one of the most common culprits behind chronic cough in kids—and it often flies under the radar because it doesn’t always look dramatic. A lot of parents expect asthma attacks to mean gasping for air or needing urgent care. But many kids with asthma don’t have obvious “attacks.” Instead, their main symptom is a persistent cough that won’t go away.
Clues it might be asthma include:
- Wheezing: A high-pitched whistling sound when breathing out.
- Shortness of breath: Especially with activity or laughing hard.
- Nighttime or early-morning cough: When airways are naturally more reactive.
- Cough with exercise or cold air: Playing outside on a chilly day, running in PE class—it triggers the cough.
Jackie explains: “Asthma doesn’t always mean dramatic attacks. Sometimes it’s just a stubborn, chronic cough that keeps coming back, especially at night or with exercise. That’s why we ask about patterns.”
Treatment focuses on reducing airway inflammation and keeping symptoms under control, so kids can do all the things they love without worry. Here’s what you can expect:
- Albuterol inhaler (a “rescue” inhaler) used as needed for quick relief during flare-ups.
- Inhaled corticosteroids (like fluticasone or budesonide) for daily use to reduce inflammation and prevent symptoms long-term.
- Identifying and avoiding triggers when possible, whether it’s pollen, pet dander, cold air, or viral infections.
Asthma plans are highly individualized—what works for one child may not be right for another. That’s why it’s so important to have an ongoing conversation with your pediatrician about your child’s symptoms, activities, and any changes over time.
Allergies and Cough Relief
Allergies aren’t just about sneezing and itchy eyes—they’re a major cause of chronic cough in kids. When kids have allergic rhinitis (whether seasonal or year-round), their nasal passages are inflamed. This leads to post-nasal drip and that constant trickle of mucus down the back of the throat that triggers chronic throat clearing and coughing.
The cough isn’t dangerous, but it can be endlessly irritating. Kids may seem fine during the day but start hacking the moment they lie down, thanks to gravity moving that drip backward.
Treatment focuses on controlling the inflammation and cutting down on triggers:
- Daily antihistamines (like cetirizine) help reduce allergic reactions and symptoms.
- Intranasal corticosteroid sprays (fluticasone, mometasone) calm down nasal inflammation at the source. Remember to check with your pediatrician or Poppins before use, as certain corticosteroid sprays are recommended for certain ages.
- Avoiding known triggers when possible—like keeping pets out of bedrooms, using dust-mite-proof bedding, or avoiding high pollen days outside.
- Keeping windows closed during peak pollen seasons and using air purifiers indoors can also make a big difference.
Jackie says: “Parents sometimes miss that allergies can cause year-round cough. Controlling the underlying allergy often fixes the cough too.”
Managing Reflux-Related Cough
Gastroesophageal reflux (GERD) can be a surprising but common cause of chronic cough in kids, especially at night.
Reflux doesn’t always mean dramatic heartburn or pain. In many kids, it’s “silent,” with stomach acid creeping up just enough to irritate the throat and airway. That leads to a chronic, dry cough or even throat clearing that seems endless.
Clues it might be reflux:
- Cough worse when lying down, thanks to gravity making reflux easier.
- Sour taste in mouth or bad breath.
- Heartburn or chest discomfort in older kids who can describe it.
- Chronic throat clearing or “frog-in-throat” voice.
Treatment for GERD-related cough always starts with lifestyle changes:
- Avoid acidic, spicy, greasy foods that trigger reflux.
- Skip chocolate and caffeine, both known to relax the valve between the stomach and esophagus.
- Elevate the head of the bed slightly to use gravity to your advantage.
- Don’t eat within 1–2 hours of bedtime to reduce nighttime reflux risk.
If these changes don’t do the trick, your pediatrician might try a short trial of a Proton Pump Inhibitor (PPI) like omeprazole or lansoprazole. The goal? Calm the acid, protect the airway, and stop that nagging cough for good.
Treating Protracted Bacterial Bronchitis
Not all chronic coughs are viral or allergic. Sometimes, a wet, productive cough that lasts over four weeks signals a bacterial infection in the lower airways, known as protracted bacterial bronchitis.
This isn’t your average cold leftover. The persistent mucus production means bacteria are thriving in the airways, and your child’s body is trying hard to clear them out. Jackie explains: “This is one of the few chronic cough causes that actually benefits from antibiotics. But we want to be sure that’s the diagnosis before prescribing.”
Treatment usually includes:
- A prescription antibiotic course (typically Augmentin) to target the bacteria.
- Saline nasal spray to clear nasal congestion and reduce post-nasal drip.
- Hydration to keep mucus thin and easier to clear.
- Plenty of rest to support the body’s healing process.
And good news for busy families: kids can typically return to school or daycare after 24 hours on antibiotics, assuming they’re feeling okay.
This is a classic case where the right diagnosis really matters. Because while most coughs don’t need antibiotics, this one often does.
Supporting Kids with Habit or Tic Cough
Here’s the curveball most parents don’t expect: not every cough has a physical cause. Habit or tic coughs are real, common, and often overlooked. They’re usually dry, repetitive, and disappear with distraction—like when the child is playing, watching a movie, or sleeping.
It’s not “faking.” It’s a reflexive, learned behavior that sticks around long after an illness clears. Sometimes it’s triggered by stress, anxiety, or even just the attention it gets. Jackie explains: “Habit cough is underrecognized but very real. The right approach can make a huge difference without any meds.”
What’s the best approach?
- Reassure your child there’s no serious illness. Removing fear is half the battle.
- Behavioral techniques like sipping water, humming, or practicing quiet breathing can help replace the cough reflex.
- Avoid repeated medical testing once this diagnosis is clear. Endless tests just reinforce the anxiety.
- Consider mental health support if the cough is persistent, stressful, or linked to anxiety or tic disorders.
The best news? With the right approach, habit cough often resolves completely.
Home Care Strategies for Cough Relief
Even if your child’s cough is stubborn, there’s a lot you can do at home to make them more comfortable—and to help them (and you) actually get some sleep.
Comfort Measures That Work
When your kid just won’t stop coughing, there are some tried-and-true methods you can use at home. These aren’t magic cures—but they’re simple, safe, pediatrician-approved ways to soothe irritated airways, ease symptoms, and support healing.
Here are some of those go-to strategies that actually work:
- Cool mist humidifier: Adds moisture to dry indoor air, helping soothe irritated airways, especially at night.
- Saline nasal spray: Safe and gentle. Loosens mucus, helps kids breathe more comfortably.
- Warm fluids: Broth, tea (decaf), warm water with lemon—helps calm the throat and thin secretions.
- Honey (for kids over 1 year old): Coats the throat and can reduce nighttime coughing.
- Hydration: Water, diluted juice—keeping them well-hydrated helps mucus stay loose.
- Gentle nose blowing or suction for little ones: Keeps nasal passages clear.
Jackie says: “Sometimes it’s the simplest things that work best. A humidifier and honey can go a long way.”
Creating a Restful Environment
When kids feel crummy and can’t stop coughing, sleep becomes a battle. But rest is essential for healing.
Here are some tips to help them sleep comfortably:
- Keep bedrooms cool and humidified (but not damp or moldy).
- Elevate the head of the bed slightly for reflux-related cough.
- Stick to a calm bedtime routine to reduce anxiety-triggered coughing.
- White noise can help mask the sound of occasional coughs and help everyone sleep better.
“A calm, cozy sleep space can make a huge difference,” Jackie explains. “You want to reduce irritation and help them relax.”
Parent FAQs About Chronic Cough in Kids
We get it—this stuff raises a million questions. Here are the most common ones parents ask us about chronic cough, answered in plain language you can actually use.
Why Does My Child’s Cough Last So Long?
It’s usually post-viral irritation. Even after a cold is gone, the airways can stay sensitive for weeks. Think of it like a scraped knee that’s still tender long after the scab. Jackie explains: “It’s incredibly common for a cough to last 3–4 weeks after a cold. That doesn’t mean it’s dangerous.”
Can Cough Be Caused by Allergies?
Absolutely. Allergies can lead to chronic drainage in the back of the throat, which triggers coughing—especially at night. Treatment focuses on controlling the allergies themselves: antihistamines, nasal sprays, and avoiding triggers when possible.
What If My Child’s Cough Is Worse at Night?
Nighttime cough can mean post-nasal drip (from allergies or colds) or reflux. Asthma is also notorious for causing nighttime cough. Your pediatrician will help figure out which is the likely cause and suggest appropriate treatment.
Is a Habit Cough Really a Thing?
Yes! Habit or tic cough is real. It’s usually a dry, repetitive cough with no underlying illness. It often disappears when the child is distracted or asleep. Treatment isn’t medicine—it’s reassurance and behavior modification. Sometimes, support from a mental health professional is helpful if anxiety or tics are involved.
When Should I Worry About My Child’s Cough?
You should see your pediatrician if:
- The cough lasts more than four weeks.
- It’s wet and productive and not improving.
- It’s associated with wheezing or shortness of breath.
- It’s waking them up regularly at night.
- They’re losing weight or seem fatigued.
Go to the ER if there are any red flag symptoms like labored breathing, blue lips, confusion, or severe dehydration.
Final Thoughts: Helping Your Child Breathe Easy
Coughs are stressful. They’re noisy, disruptive, and they can make even seasoned parents question themselves.
But most chronic coughs in kids have clear, treatable causes once you know what to look for. The key is understanding what’s normal, recognizing the warning signs, and partnering with your pediatrician to get the right care.
And you don’t have to figure it all out alone. Sign up for Poppins today to get 24/7 access to smart, compassionate pediatric care—so you never have to guess what’s serious, what can wait, or what to try next.

