Written by: Jenn Schoen, Pediatric Sleep Consultant
If you’re reading this, you’re probably tired. The kind of tired that makes you open the dishwasher and wonder why your phone isn’t charging inside it.
Let’s start with the most grounding truth: your newborn’s sleep is not broken, and you’re likely not doing anything wrong.
Newborn sleep is biologically fragmented, inconsistent, and often feels unpredictable. Their brains, hormones, and internal body clocks are still wiring themselves together, and it takes time for things to click. As Jenn Schoen, a certified pediatric sleep consultant at Poppins, puts it: “Nothing about newborn sleep is a failure on your part. It’s biology doing exactly what biology is supposed to do.”
This guide walks you through what typical newborn sleep looks like, why day–night confusion happens, how melatonin and cortisol shape sleep patterns, and what you can realistically do to support better rest in these early months. And if you’re considering a sleep consulting package with Poppins, this will give you the “why” behind our approach to supporting healthy, sustainable sleep habits.
What “Normal” Newborn Sleep Really Looks Like
Newborns and young infants have immature sleep systems that develop gradually. Their short sleep cycles, frequent feeds, and inconsistent patterns aren’t problems—they’re protective adaptations that serve an evolutionary purpose.
Jenn explains: “When parents tell me ‘She wakes every hour, I must be doing something wrong,’ I always remind them that newborns wake often because their sleep system is still developing. Nothing about that pattern is a sign of failure or that something is wrong.”
Sleep in the First Year: the Big Picture
If you’re wondering what “normal” even means when it comes to baby sleep, this quick outline can help put everything in perspective.
- 0–3 months: In these early months, babies often sleep 14–17 hours total, but the sleep is irregular—naps are unpredictable, nights are broken, and day–night confusion is completely normal.
- 4–12 months: As babies grow, total sleep shifts to about 12–16 hours per day, with naps becoming more consistent and nighttime sleep stretching into longer, more predictable blocks.
These ranges are helpful guideposts, not scorecards. Every baby sits somewhere on the spectrum of what’s typical.
Why Newborns Struggle With Day–Night Confusion
If your newborn sleeps beautifully during the day and then wants to party at 2 a.m., you’ve met day–night confusion—a universal newborn rite of passage. It happens for a few very real, very biological reasons:
- Their circadian rhythm isn’t developed yet. Babies aren’t born knowing night from day because they don’t have a functioning internal body clock at birth. In the womb, there were no light cues to help them build one, so their sleep patterns are naturally round-the-clock and inconsistent in the early weeks.
- Their in-utero habits were flipped. During pregnancy, your daytime movement rocked your baby to sleep, while nighttime stillness often meant they had more room to move—so they were awake and active. That rhythm carries over after birth, making nighttime alertness completely normal for newborns.
- Their melatonin levels are still very low. Newborns don’t produce meaningful amounts of melatonin—the hormone that signals nighttime sleepiness—until around 3 months of age. Without strong melatonin cues, they don’t have the biological nudge to sleep longer stretches at night.
Jenn explains it simply: “Babies aren’t born knowing day from night. They usually figure it out within 2–8 weeks, but you can help move the process along by keeping daytime bright and engaging and nighttime dark, cool, and quiet.”
Helping Your Baby’s Circadian Rhythm Develop
You don’t “train” a newborn in the traditional sense—honestly, there’s nothing to train yet. What you can do is offer simple, repeated cues that help your baby’s still-developing circadian rhythm start to make sense of the world. Think of it as gently narrating the difference between day and night until their biology catches up.
How to Support Your Newborn’s Circadian Rhythm During the Day
Your newborn’s internal body clock learns best through contrast, so daytime is your chance to show them, “This is when we’re awake.”
- Keep the lights bright. Let natural sunlight pour in or flip on the lights. Your baby’s brain is soaking up those light cues—even if their eyes are barely open and they look vaguely unimpressed. Jenn adds, “After your baby learns day from night, blackout curtains will be your nap-time best friend. But in the early weeks, keep daytime bright to help their internal clock take shape.”
- Talk, play, and let normal noise happen. No need to tiptoe around like you’re living with a very tiny, easily startled celebrity. Everyday household sounds help signal, “We’re in awake-mode now.”
Creating a Nighttime Environment That Helps Your Newborn Sleep
Nighttime is your opportunity to communicate, “Okay buddy, this is the part where we rest.”
- Dim the lights. Even a subtle shift toward darkness tells their little brain, “We’re winding down.” Jenn adds, “Begin dimming the lights a couple of hours before bedtime. It gently eases your little one into the evening so bedtime doesn’t feel abrupt.” If you need some light for late night feedings, try a red night light, which does not impact melatonin production.
- Move slowly and calmly. Think gentle, predictable motions to limit stimulation, which can work against sleep.
- Follow a quiet, consistent bedtime or pre-sleep routine. It doesn’t need to be elaborate. A short sequence—feed, change, sleep sack, lullaby—is enough to cue their body that sleep is next.
These simple tactics are biologically aligned signals that help your baby’s circadian rhythm gradually come online.
Melatonin, Cortisol, and Your Baby’s Sleep Hormones
Sleep isn’t just about being tired—it's a delicate dance between two major hormones: melatonin and cortisol. In the newborn period, these hormones are still getting their act together, which is why sleep can feel so unpredictable. Understanding how they work (and when they don’t) can help you make sense of your baby’s patterns.
How Melatonin Works in Newborns and Why It Affects Baby Sleep
Melatonin is the quiet hero of nighttime sleep. It’s the hormone the brain releases in response to darkness—telling the body, “It’s time to settle, rest, and stay asleep.”
But newborns? They produce virtually no melatonin. In the womb, they never experienced day versus night, so their bodies didn’t learn to create those sleep–wake signals. Around 3 months, melatonin finally begins to rise, and that’s when nighttime sleep slowly starts to organize, and they begin sleeping longer stretches.
As Jenn explains: “When sleep starts to feel even slightly more predictable in that 10–14-week range, it’s usually melatonin settling into its rhythm.”
This shift doesn’t mean your baby will suddenly sleep through the night, but it does mean their body is starting to understand nighttime in a way it simply couldn’t before.
How Cortisol Affects Baby Sleep and Why Overtiredness Causes Spikes
If melatonin is the gentle nudge toward sleep, cortisol is the hormone that keeps us awake, alert, and ready to respond. Babies are born able to produce cortisol—they need it to help regulate hunger, alertness, and survival cues. But here’s the catch: they can’t regulate cortisol well yet.
So when they get overtired? Their little bodies release cortisol at the worst possible moment (e.g. bedtime), making it significantly harder for them to fall or stay asleep. That’s why we place so much emphasis on sticking to age-appropriate wake windows, which help to prevent overtiredness.
Jenn explains it like this: “If your baby has stretched past their wake window and suddenly seems full of energy, they’ve likely slipped into overtired territory—and that ‘burst’ is actually a cortisol spike.”
This knowledge isn’t meant to convince you that sticking to a rigid schedule is the answer—it’s more about recognizing that newborn behavior is rooted in biology. When you work with your baby’s hormonal rhythms instead of against them, everything feels smoother and more manageable.
Working With Your Baby’s Biology: Calm, Cool, and Dark
Here’s the part most parents find frustrating: you can’t force newborn sleep to organize itself before the hormones are ready. But you can create conditions that stack the deck in your baby’s favor. Think of it as partnering with your baby’s biology rather than trying to override it.
Jenn advises parents: “When it comes to baby sleep, think calm, cool, and dark. You can’t control your baby’s biology, but you can control their environment—and that goes a long way toward helping everyone sleep better.”
Part 1: Creating a Calm Environment for Your Newborn
A calm body supports a calm brain. Before sleep, try:
- A predictable wind-down routine: It doesn’t need to be fancy—feed, change, sleep sack or swaddle, lullaby or book. These steps cue your baby that sleep time is coming.
- Reduce external stimuli 60–90 minutes before sleep: dim the lights, lower the noise, and keep activity minimal. This helps your baby’s body transition into a sleep-ready state.
- White noise: This helps settle your baby’s nervous system and drowns out the “Did someone just drop a pan?” moments.
These cues help your baby gently shift out of “take in the world” mode and into “time to rest” mode.
Part 2: How a Cool Sleep Environment Helps Your Newborn Sleep
Temperature makes a remarkable difference in sleep quality—even in newborns.
Aim for:
- A room around 68–72°F: Cool enough to support melatonin but warm enough for safe sleep.
- Breathable sleepwear: Cotton or bamboo layers help regulate temperature. The American Academy of Pediatrics (AAP) recommends dressing your baby in one more layer than what you’d be comfortable in.
- A sleep sack or swaddle instead of blankets: Keeps your baby safely warm without loose bedding. Remember: Switch from a swaddle to a sleep sack as soon as your baby begins showing signs of rolling.
Part 3: Why Dark Sleep Environments Support Melatonin Production
Light is one of the strongest cues for the circadian rhythm—even long before melatonin fully matures. Because light suppresses melatonin, reducing light exposure 60-90 minutes before bedtime helps your baby’s sleepiness hormone rise as bedtime approaches.
At nighttime or before naps:
- Dim the lights well before sleep: Think warm, soft lighting, not overhead LEDs.
- Once day-night confusion is resolved, use blackout curtains during naps: Even a sliver of daylight can be stimulating.
- If you need a nightlight, choose a dim red light: Red light interferes the least with melatonin.
Combined, calm, cool, and dark tell your baby, “Okay, the world is slowing down now.”
How to Use Age-Appropriate Wake Windows to Improve Baby Sleep
Using age-appropriate wake windows is one of the most effective ways to improve newborn and infant sleep. Wake windows help prevent your baby from staying awake too long, which is when overtiredness and cortisol spikes make it harder for babies to fall asleep and stay asleep. When you follow wake windows by age, you’re aligning sleep pressure, melatonin, and cortisol in a way that naturally supports smoother naps and longer nighttime stretches.
Jenn often reminds families that wake windows aren’t about rigid schedules—they’re about staying within the range your baby’s biology can handle. Babies build sleep pressure quickly, which means they can’t comfortably stay awake for long periods. As Jenn explains: “Wake windows are one of the most powerful tools we use. Get the timing right, and sleep feels smooth. Miss it, and everything becomes harder.”
Understanding Baby Wake Windows by Age
Use these wake window ranges to time naps and bedtime so your baby builds enough sleep pressure—without slipping into overtiredness.
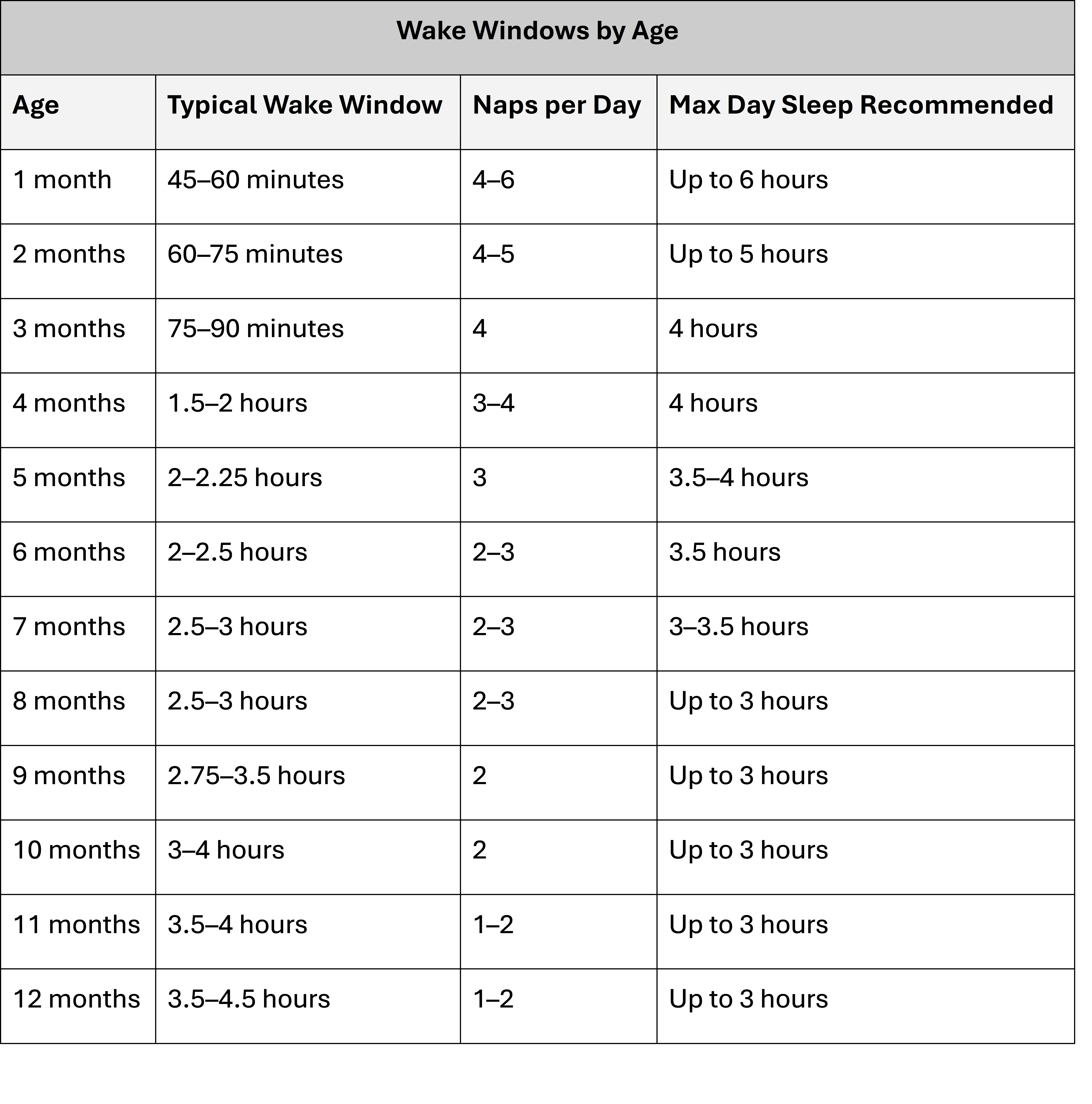
Pairing age-appropriate wake windows with your baby’s sleepy cues—and creating a calm, cool, dark sleep environment—gives your newborn the best chance of settling easily, transitioning between sleep cycles, and gradually developing more predictable, consolidated sleep as their hormones mature.
Recognizing Baby Sleep Cues Before Overtiredness Hits
While wake windows offer a general guide to when your little one will need rest, sleepy cues are the signals that say “Ok, now I’m ready”. Sleep cues look like:
- Yawning
- Rubbing eyes
- Brief, sudden fussiness
- Zoning out or staring into space
- Turning away from stimulation
- Redness around the eyebrows
These are your gentle nudges to begin the routine and allows you to sync sleep opportunities with your baby’s natural rhythm.
Frequently Asked Questions About Newborn Sleep
These are some of the most common questions parents ask when trying to understand newborn sleep, day–night confusion, wake windows, and what “normal” truly looks like in the first few months.
Why Does My Newborn Wake Up So Often at Night?
Frequent waking is typical in newborns. Their sleep cycles are short—often 40 to 50 minutes—and they spend about half of that time in REM sleep, which is lighter and more active. These short, fragmented sleep cycles make it easier for newborns to wake when hungry, uncomfortable, or overstimulated. This is a biologically protective pattern, not a sign that anything is wrong.
When Will My Baby’s Sleep Start to Improve or Feel More Predictable?
Many parents notice sleep starting to feel more organized around 10–14 weeks, when melatonin production increases and the baby circadian rhythm begins to develop. This shift helps nighttime sleep gradually consolidate, even though frequent waking is still developmentally normal.
How Can I Fix Newborn Day–Night Confusion?
Day–night confusion improves when you give your baby consistent environmental cues. During the day, keep lights bright and engage in normal activity; at night, keep things dim, quiet, and calm. This contrast helps regulate the developing circadian rhythm, teaching your baby the difference between daytime wakefulness and nighttime sleep.
What Are Age-Appropriate Wake Windows for Newborns and Young Infants?
Wake windows vary by age: around 45–60 minutes at one month, slowly increasing to 75–90 minutes by three months. Following wake windows helps balance sleep pressure, prevents overtiredness, and reduces cortisol spikes that can make settling difficult.
How Do I Know If My Baby is Overtired?
Signs of overtiredness include intense fussiness, difficulty settling, a “wired” or frantic look, short naps, and frequent night waking. These behaviors often reflect cortisol spikes, which happen when babies stay awake longer than their developmental capacity.
Should Newborns Have a Bedtime Routine?
Yes—a simple, predictable bedtime routine supports melatonin production and helps your baby’s nervous system wind down. This could include a feed, diaper change, swaddle, dim lights, white noise, and a brief lullaby. Routines don’t need to be elaborate; consistency is what matters.
How Much Should My Newborn Sleep During the Day Versus at Night?
Newborns (0–3 months) typically sleep 14–17 hours in 24 hours, with sleep distributed irregularly across day and night. Their circadian rhythms are not yet developed, so unpredictable patterns are expected. Daytime naps gradually consolidate and nighttime sleep lengthens as babies move into the 4–12 month range.
Why Does My Baby Get Fussy or Hysterical Right Before Falling Asleep?
Fussiness is your baby’s way of saying, “I’m getting tired.” It’s one of the sleep cues that we tell parents to be on the lookout for. If that early fussiness is missed, babies can move into overtiredness quickly—and that’s when the crying becomes intense or “hysterical”. At that point, cortisol is high and falling asleep feels much harder for them.
Is It Normal for Newborns to Twitch, Grunt, or Move a Lot While Sleeping?
Yes. Newborns spend a large portion of their sleep in active REM sleep, which is marked by irregular breathing, facial movements, twitching, and “busy” sleep. REM is critical for brain development, memory formation, and neural growth.
Does Poor Sleep Affect My Baby’s Development?
Chronic and significant sleep disruption can affect a baby’s development—but it’s important to understand what “poor sleep” truly means. Sleep needs and sleep duration vary widely between 0–12 months, and frequent night waking or short naps are normal parts of early development.
What’s more concerning is persistent overtiredness, very fragmented sleep that doesn’t improve over time, or patterns that lead to insufficient total sleep for a baby’s age. In those cases, research shows that emotional regulation, cognitive processing, and physical growth can be impacted, since deep sleep supports growth hormone release and REM sleep helps build memory pathways. Sleep challenges can also increase family stress and maternal depressive symptoms.
Most newborn sleep variability is normal—and not harmful. Concern arises when sleep is consistently insufficient for a baby’s developmental stage.
How Poppins Sleep Consulting Can Support Your Family
Understanding newborn sleep biology is empowering—but putting it into practice when you're sleep-deprived can feel overwhelming. You don’t need a color-coded spreadsheet or a hyper-strict schedule. You need a plan that works with your baby’s biology and your family’s reality.
That’s where Poppins comes in.
Our personalized sleep consulting includes:
- A full sleep assessment and plan tailored to your baby’s age and temperament
- Same-day coaching support through secure messaging
- Step-by-step guidance grounded in developmental science
- Techniques that support sleep without pushing your baby before they’re ready
- A certified pediatric sleep consultant walking with you through every change
Whether you’re dealing with day–night confusion, short naps, bedtime meltdowns, or constant night waking, we’ll help you understand the why—and create a plan that feels gentle, doable, and effective.
If you’re ready to feel more confident, more rested, and more supported, Poppins sleep consulting is here to help you get there.

