You know the sound—the yell from the yard, the 'thump' of a fall, the "I need help getting up” moment that sends your heart rate through the roof.
Take a deep breath. Sprains and strains are part of the parenting gig, but knowing how to assess, treat, and monitor them can make you feel so much more prepared. Let’s break it all down—no panic required.
Understanding Sprains and Strains in Kids
Kids play hard, and injuries happen. But not all injuries are the same. Before you reach for the ice pack or rush to urgent care, it helps to know whether you're dealing with a sprain or a strain—and what that means for your child's care plan.
What Is a Sprain?
A sprain is an injury to the ligaments—the strong, fibrous tissues connecting bones at a joint. Sprains often happen when a child twists, lands awkwardly, or falls suddenly.
Signs of a sprain in kids include:
- Swelling around the joint.
- Bruising or discoloration.
- Pain that worsens with movement or weight bearing.
“Sprains can look dramatic at first because of swelling and bruising,” says Poppins pediatric nurse practitioner Jessica Kimmes. “But with the right home care, many heal well without much intervention.” *Ankle sprains are a common sports injury in young children, accounting for 10 to 30% of all sports-related injuries.*
What Is a Strain?
A strain affects muscles or tendons—the tissues that connect muscles to bones. Strains often result from overuse (like playing sports without enough warmup) or repetitive motions.
Signs of a strain include:
- Soreness or stiffness.
- Pain with specific movements.
- Limited range of motion in the affected area.
Kimmes notes, “Parents often notice strains in kids who’ve been extra active after a break—like the first week of soccer practice.”
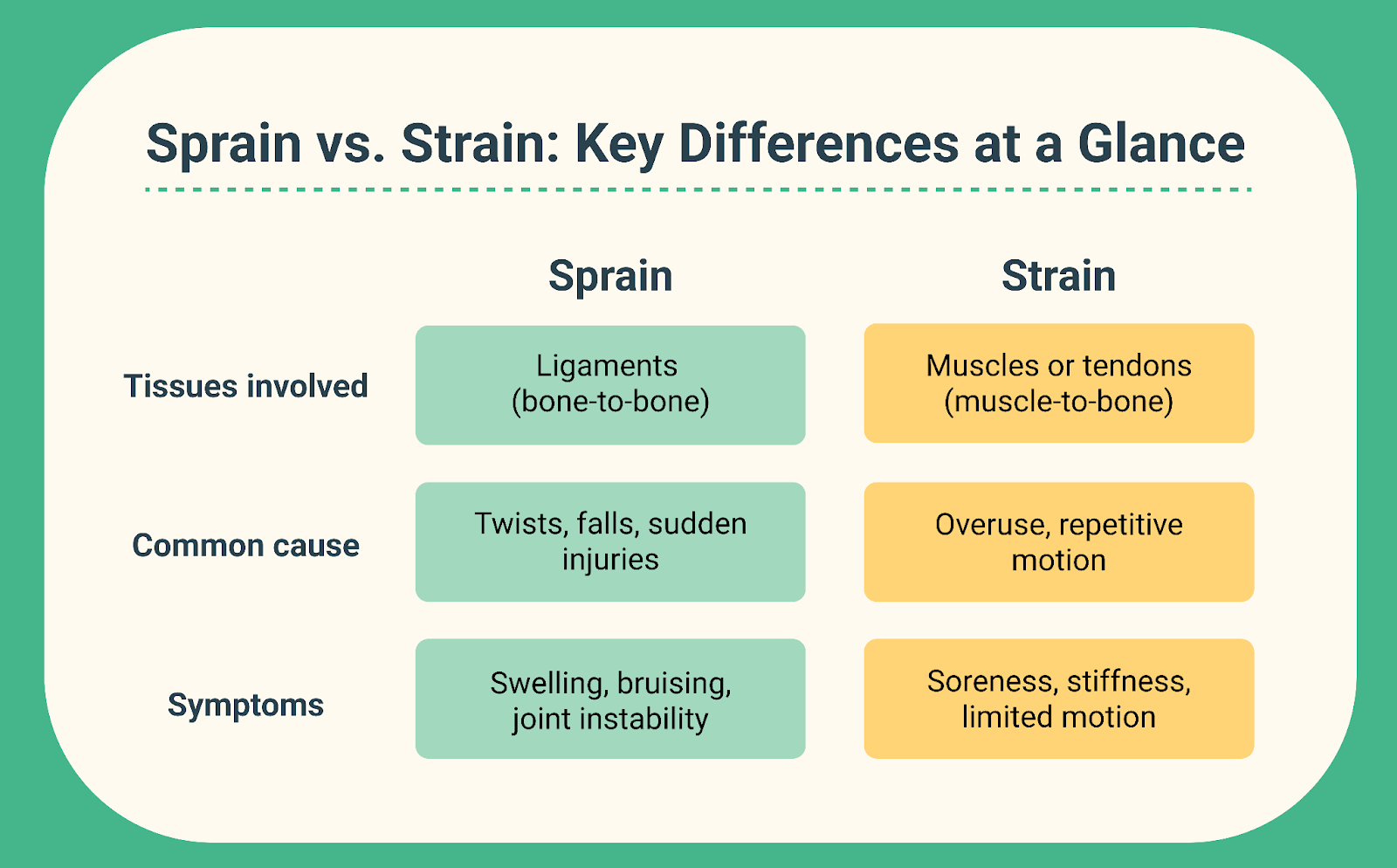
Sprain vs. Strain Cheat Sheet
Still not sure how to tell the difference between a sprain and a strain? Use this simple cheat sheet.
Assessing Your Child’s Injury
Before you start treating, take a minute to really assess what happened. The story of the injury—and your child’s current symptoms—can help you figure out if it’s safe to treat at home or if you need professional evaluation.
How Did It Happen?
Ask your child (and observe if they’re little):
- Was it a sudden twist, fall, or impact? (More likely a sprain.)
- Was it from repeated activity over time? (More likely a strain.)
Knowing how the injury occurred can guide next steps and help rule out more serious injuries like fractures or concussions.
Key Questions to Ask
These questions help you gauge severity and plan care:
- Any swelling or bruising? Significant swelling may suggest a sprain or even a fracture.
- Hearing or feeling a “pop”? A “pop” sound or sensation is often linked with ligament injury (sprain) or even a more severe tear.
- Can they move it normally? Limited range of motion suggests a more serious injury.
- Weight bearing on both legs? Inability to put weight on an ankle or leg may indicate a fracture.
- Numbness or tingling? Could suggest nerve involvement or significant swelling cutting off circulation.
- Head impact? Always consider concussion if there was a fall or hit to the head.
Kimmes advises: “These questions aren’t just a checklist—they’re your triage tool. They help you decide whether you can manage at home or need medical input.”
Red Flags Requiring Urgent Care
If you see any of these, seek professional evaluation immediately:
- Can’t walk or move the injured area: If your child can’t walk at all or refuses to move the injured limb, it might be a broken bone or a more serious injury. Ask them to try putting some weight on it gently. If they truly can't bear any weight or there is severe pain that limits motion, get it checked.
- Pain right on the bone: Press gently along the injured area. If your child has sharp, strong pain right on the bone (not just general soreness in the muscles), it could be a sign of a fracture and should be evaluated.
- Pain that doesn’t get better after a day or two: If your child’s pain isn’t improving, or it’s actually getting worse after 24–48 hours of home care, it’s time to have a doctor take another look.
- Joint pain or swelling without an obvious injury: If your child has joint pain or swelling but didn’t have a clear fall or twist, it could be another condition that needs medical evaluation, like an infection or arthritis.
Kimmes adds, “If a child refuses to use the limb at all or pain is escalating despite ibuprofen, that’s your cue to get help.”
When to Consider an X-Ray or Imaging for Your Child’s Injury
Not every bump, twist, or fall needs an X-ray. In fact, avoiding unnecessary imaging is a good thing—it reduces radiation exposure and stress for your child. But some injuries really do need that closer look. Knowing when to consider an X-ray can help you make confident decisions about care.
Jessica Kimmes, Poppins pediatric nurse practitioner, explains: “Parents often ask, ‘Should we go for X-rays?’ We want to balance being cautious with avoiding unnecessary trips. There are clear guidelines to help.”
How to Use the Ottawa Ankle Rules for Kids
The Ottawa Ankle Rules are a set of evidence-based criteria used by clinicians to decide if an ankle X-ray is needed. They’re simple enough for parents to use at home to guide next steps.
When to consider an ankle X-ray:
- Bone tenderness: Press gently on the lower part of the ankle (about 2–3 inches above where the foot meets the ankle) on both the inside and outside. If your child feels sharp pain right on the bone when you press, that’s a sign they might need an X-ray. You’re looking for specific, strong pain on the bone itself, not just general soreness or muscle ache around it.
- Inability to bear weight (both immediately and in the clinic or at home): Ask your child to try taking four steps on the injured foot. If they can’t put any weight on it or collapse from pain, that’s a strong indicator for imaging.
“We use these rules in the clinic to decide if an X-ray will help,” says Kimmes. “They’re easy for parents to try at home too. They can save families unnecessary trips while catching important injuries.”
Extra tip for parents: Don’t force a child to walk if they’re in severe pain—ask them gently to test weight bearing if they're comfortable trying.
Signs Your Child May Have a Fracture Beyond the Ankle
While the Ottawa Rules focus on ankles, fractures can happen anywhere. Here’s how to spot red flags that may warrant imaging for other body parts.
- Toddler’s fracture risk with knee or ankle pain: Even a mild-looking twist can cause a subtle hairline fracture in toddlers. Look for new limping or refusal to walk after a seemingly small fall. Other signs include persistent crying or guarding the leg.
- Pain directly over bone: Press gently along the whole injured area. If your child feels sharp, strong pain right on the bone in one specific spot, that could mean a broken bone. General soreness in the muscles around it is less worrisome—what you’re looking for is clear, pinpoint pain right on the bone itself.
- Swelling that’s significant or getting worse: Keep an eye on swelling that doesn’t get better after 1–2 days of rest, ice, compression, and elevation (RICE). Watch for skin that looks tight or shiny, or bruising that keeps spreading.
- Visible bending or crooked appearance: If the injured area looks bent the wrong way or crooked, that’s a clear sign to see a doctor right away.
Head Injuries and the Need for Imaging
Don’t forget to check the head if your child took a big tumble! Falls from playground equipment, bikes, beds, or couches often involve head impacts—even if your child doesn’t mention hitting their head. Kids may underreport pain, be distracted by other scrapes, or simply forget.
Always ask them directly: “Did you hit your head?”
It’s important to know when a head injury can be safely watched at home—and when it needs professional evaluation or imaging (like a CT scan). Imaging is usually reserved for specific concerning signs, to avoid unnecessary radiation exposure in children.
Here are signs to watch out for in case of a possible concussion or serious head injury:
- Nausea or repeated vomiting. One isolated episode of vomiting after a fall is not always alarming, but repeated vomiting can indicate pressure or bleeding in the brain.
- Confusion or trouble answering simple questions. Disorientation, memory gaps about the fall, or trouble understanding you can suggest a brain injury.
- Unusual sleepiness or difficulty waking. Sleepy kids are common after crying and exhaustion—but if your child is hard to rouse or you can’t keep them awake, seek care immediately.
- Loss of consciousness, even brief. Any blacking out, even for seconds, increases the chance of a concussion or more serious injury.
- Changes in behavior or extreme irritability in young kids. Babies and toddlers can’t always tell you they have a headache or feel dizzy. Watch for inconsolable crying, refusing to eat, being “just not themselves,” or sudden big personality shifts.
- Severe or worsening headache. A mild headache is common after a bump, but severe or increasing pain can be a red flag.
- Balance or coordination problems. Trouble walking, staggering, or clumsiness beyond the usual post-fall fright suggests brain involvement.
Call your pediatrician or go to the emergency department if you see any of these symptoms. For severe signs (like unresponsiveness or repeated vomiting), call 911.
Kimmes warns, “Concussions can be sneaky. If a child fell and hit their head—even if they seem okay at first—watch them closely for evolving symptoms. Problems can appear hours after the injury.”
Bottom Line: Most minor head bumps don’t need imaging, but it’s critical to know the warning signs. When in doubt, call your pediatrician for guidance. They’ll help decide if your child can be monitored at home or needs further evaluation.
When in Doubt, Check with Your Pediatrician or Poppins
If you’re uncertain about whether imaging is needed, don’t hesitate to ask for help.
- Your pediatrician or a Poppins clinician can guide you through the assessment virtually.
- They’ll help you decide if an X-ray is recommended or if it’s safe to monitor at home.
- Early consultation can also help rule out other causes of joint pain, like infections or arthritis.
Kimmes says, “We’d always rather you ask than worry alone. We’re here to help parents make these calls with confidence.”
At-Home Treatment Plan for Sprains and Strains in Kids
If you’ve ruled out urgent red flags—like inability to walk, severe pain, or signs of a break—you can often manage your child’s sprain or strain at home. But "home care" doesn’t mean doing nothing. A thoughtful approach can reduce swelling, control pain, and help your kid bounce back faster.
“Parents often worry they’ll do something wrong,” says Kimmes. “But with a few simple strategies, you can really support your child’s healing.”
How to Use the RICE Method for Sprains and Strains
The RICE method is a classic, evidence-based approach to treating mild-to-moderate sprains and strains at home. It helps control swelling, reduce pain, and promote healing in the first critical days.
Rest
Have your child take it easy for the first few days. Avoid running, jumping, or rough play. Encourage them to rest the injured area, but don’t keep it completely still if they can move it comfortably. Gentle movement is actually helpful if it doesn’t hurt.
Ice
To help reduce swelling and numb pain after an injury, place a cold pack on the affected area for 15 to 20 minutes every 2 to 3 hours during the first day or two. Always wrap the ice pack in a towel or cloth to prevent direct contact with the skin and avoid frostbite. If your child doesn’t tolerate the cold well, you can try using a cool, damp cloth as a gentler alternative.
Compression
Wrap the injured area with an elastic bandage to help control swelling, making sure it’s snug but not too tight—you should be able to slip a finger underneath the wrap. Check your child’s fingers or toes beyond the bandage frequently to ensure they stay warm and maintain their normal color, confirming that circulation is not restricted.
Elevation
Try to keep the injured area raised above the level of the heart as much as possible.
- For ankles or legs: prop them up on pillows while sitting or lying down.
- For arms: rest them on a pillow or the arm of a chair.
Elevating the injury allows gravity to help drain excess fluid in the area away, which should reduce swelling.
Kimmes notes, “Even little kids can learn ‘RICE’ with a fun chart or checklist. It helps them feel involved and less scared.”
Ice vs Heat for Kids’ Sprains and Strains
Timing and safety are essential when using temperature therapy to treat sprains and strains in children.
Ice is best used during the first 24 to 48 hours after an injury. It helps reduce swelling, inflammation, and pain. Apply a cold pack for 15 to 20 minutes at a time, making sure there’s at least an hour between sessions. Always use a barrier like a towel or cloth to avoid direct contact with the skin, which can cause frostbite.
Heat can be introduced after the initial 48 hours, once swelling has gone down. Warm compresses or heating pads promote circulation - which helps improve healing and ease lingering stiffness. Apply heat for 10 to 15 minutes at a time, and always test the temperature first to avoid burns—this is especially important for younger children.
“Parents often skip heat entirely, but it really helps with stiffness after the acute phase,” Kimmes says.
Pro Tip: Teach older kids to set a timer so they don’t overdo it!
Safe Pain Relief for Kids with Sprains and Strains
Pain control is an important part of home care. When used appropriately, over-the-counter medications can make a big difference.
Ibuprofen (Motrin or Advil)
Ibuprofen is often a good choice for kids with sprains and strains because it helps with both pain and swelling. Here’s what to know:
- It works well to relieve pain and reduce inflammation.
- Follow the weight-based dosing instructions on the package or as directed by your provider, usually every 6 to 8 hours.
- By lowering swelling, it can make it easier for your child to move the injured area.
Acetaminophen (Tylenol)
Acetaminophen is another option to help manage your child’s discomfort. Keep in mind:
- It’s effective for relieving pain but doesn’t help with swelling.
- It can be a good choice if your child can’t take ibuprofen or if you want an alternative for pain relief.
Important safety tips: When giving medicine for pain or swelling, use only one type at a time unless your pediatrician tells you it’s okay to combine them. Always choose the correct children’s formulation—avoid using adult versions without specific guidance from your provider. Most importantly, never give more than the recommended dose to keep your child safe.
Encouraging Gentle Movement and Exercise After Injury
One of the biggest mistakes? Keeping kids totally still for too long. While rest is important in the first days, gentle movement is critical to avoid stiffness and support circulation.
Pro tip: little kids around 1-3 years old will only move if it feels ok for them, so you don't have to worry if they're back to playing 'too much'. If they’re up and going, that means they're good to go.
Use the Limb Carefully
Help your child start using the injured area again, but do so gently and with caution. Keep these tips in mind:
- Encourage them to move it within pain limits.
- Avoid forcing any motion.
- Let them decide how much feels safe—but supervise.
Gentle Range-of-Motion Exercises
Once pain starts to improve, try simple movements to keep the joint flexible. You can do things like:
- Slowly bend and straighten the joint.
- Make “circles” with ankles or wrists if pain allows.
- For knees or elbows, practice gentle flexion and extension.
Light Activities
When your child is ready, introduce easy activities to keep them moving without overdoing it:
- Walking on flat surfaces if they can bear weight comfortably.
- Easy seated stretching.
- Simple balance games or seated ball rolling for younger kids.
“Movement helps kids heal faster—but it has to be the right kind of movement,” says Kimmes. “We want gentle, controlled, and pain-free activities.”
Keep an eye out for signs that your child may be overdoing it or needs more support. These signs may include sharp pain with movement, swelling that worsens after activity, or reluctance to use the limb at all after trying.
If you see these signs, scale back activity, ice, and consider follow-up with your provider.
Bottom line? A thoughtful, balanced home plan can help your child recover faster and reduce the chance of re-injury. And if you’re ever unsure—Poppins clinicians are here 24/7 to help you figure it out.
When to Return to Sports and Activities
Your child may be desperate to get back on the field or playground—but this is one of those times you have to be the cautious adult. Even when a sprain or strain seems better, rushing recovery can mean re-injury and even longer on the sidelines. It’s all about finding that balance between safe activity and enough healing time.
Wait for Full Recovery
Most strains and sprains will feel better after two weeks, though more serious muscle strains may take several weeks to months. Before you green-light sports or high-impact play, however, your child should be completely symptom-free for at least 24–48 hours. That means:
- No pain at rest or with gentle movement.
- Full, pain-free range of motion in the joint or limb.
- No swelling or visible bruising that’s worsening.
- Ability to walk or bear weight normally, without limping.
Encouraging them to ease back in gradually—think light jogging before sprinting, gentle kicking before full-on soccer practice—reduces the risk of setbacks.
“If they’re limping, they’re not ready for soccer yet,” warns Kimmes. “Kids love to push through, but you have to hold the boundary for them. A couple more rest days now saves them weeks later.”
For more severe injuries—like significant sprains with major swelling or strains that sidelined them completely for days—consider an in-person assessment before returning to sports. Your pediatrician can check the range of motion, pain response, and strength to clear them safely.
Watch for Setbacks
After your kiddo returns to the field, be on the lookout for signs they need to slow down or see the doctor:
- Pain returning with activity: If they’re fine walking but limping after practice, it’s too soon. Reduce activity level, ice, rest, and consider follow-up.
- Swelling or bruising coming back: A sign the tissue isn’t fully healed.
- Symptoms not improving after 3–5 days: Ongoing pain or swelling suggests it needs reassessment.
It’s also normal for kids to under-report pain because they’re excited to get back. Check in with them honestly—ask about soreness after practice or the next morning, and watch how they move when they think you're not looking.
Kimmes says, “I always tell parents: The goal isn’t just getting them back to play, but keeping them there. That takes patience and watching for those early warning signs.”
Bottom line? Don’t let the excitement of return-to-play overshadow your child’s comfort and safety. A few extra days of healing can make all the difference.
Follow-Up with Poppins
Our goal at Poppins is to make sure you don’t feel alone when managing your child’s injury.
Personalized Action Plan
Poppins clinicians provide:
- A step-by-step plan tailored to your child.
- Guidance on medications, ice/heat schedules, and safe activity levels.
- Tips on monitoring for complications.
Scheduled Check-Ins
We don’t just leave you hanging:
- 24-hour follow-up texts to check on progress.
- Imaging referrals if your child’s condition doesn’t improve or suggests fracture.
Kimmes says, “Our families love knowing we’ll check back in. It takes the guesswork out of when to worry.”
FAQs About Sprains and Strains in Kids
These are some of the most common questions we hear from parents worried about sprains, strains, and “maybe it’s broken?” moments. Let’s walk through what you really need to know.
How Can I Tell If It’s a Sprain or a Break?
This is the question we get most often.
A sprain usually results from a twist or fall that overstretches or tears ligaments. You’ll often see:
- Swelling.
- Bruising.
- Pain that may worsen with movement or weight bearing.
- Some (though limited) ability to move or use the joint.
A fracture (broken bone) is typically more severe. Watch for:
- Intense pain that doesn’t ease with rest or meds.
- Significant swelling or obvious deformity.
- Inability to bear weight at all.
- Numbness or tingling beyond mild “fall asleep” feelings.
If in doubt, err on the side of caution and get it checked. An X-ray may be needed to rule out a break.
See When to Consider an X-Ray for details on assessing for fractures.
Should I Go to Urgent Care or The ER?
It’s normal to wonder: Is this an ER-level problem? Or can we wait for clinic hours?
Head to urgent care or the ER if:
- Your child can’t bear any weight on the leg or walk four steps.
- There’s severe pain not responding to ibuprofen or acetaminophen.
- The injured area looks deformed or significantly misaligned.
- There’s numbness, tingling, or loss of sensation that doesn’t improve quickly.
- They hit their head and show signs of concussion (vomiting, confusion, excessive sleepiness, loss of consciousness).
If you’re unsure, medical professionals will help assess and refer as needed.
Check Red Flags Requiring Urgent Care for a full checklist.
How Long Will Recovery Take?
The answer depends on the severity of the injury.
- Mild sprains/strains: Often improve in a few days to 2 weeks with RICE and gentle movement.
- Moderate to severe sprains/strains: May take 4–6 weeks or more.
- Fractures: Varies widely depending on the bone and the break, but typically 4–8 weeks or longer.
Healing is faster with early, appropriate care—and following return-to-play guidance carefully.
See When to Return to Sports and Activities for safe timelines.
Is It OK For My Child to Walk on a Sprain?
In many cases, yes—but it depends on severity. If your child can comfortably bear weight, encourage gentle use of the limb. Movement helps circulation, reduces stiffness, and speeds healing.
However, we encourage parents to follow these recomendations:
- Don’t push through severe pain.
- Avoid high-impact activities or sports until cleared.
- Consider using crutches for partial weight bearing if advised.
Kimmes notes, “Kids bounce back quickly, but they also push limits. It’s important to supervise them to avoid re-injury.”
See Encouraging Gentle Movement for safe exercise ideas.
How Do I Know If My Child Needs an X-ray?
If you’re unsure whether your child needs an X-ray, you can use these guidelines at home:
- Check for bone tenderness (especially along the lower leg for ankle injuries).
- See if they can bear weight (four steps).
- Watch for deformity or significant swelling.
If they can’t do these, an X-ray is often recommended to rule out fracture.
Read Using the Ottawa Ankle Rules and Considering Fractures for step-by-step assessment tips.
What’s the Best Way to Ice or Heat an Injury?
When it comes to using ice and heat for sprains and strains, timing is key:
- Ice: Use in the first 24–48 hours to reduce swelling. Apply for 15–20 minutes every 2–3 hours. Always wrap ice in a cloth; never apply directly to skin to prevent frostbite.
- Heat: After 48 hours, helps circulation and eases stiffness. Use warm compresses or gentle heating pads for 10–15 minutes at a time.
“Parents often forget to switch to heat after icing,” Kimmes explains. “But it’s really helpful once swelling is controlled.”
See Ice vs Heat for full instructions.
Which Pain Medications Are Safe For Kids?
Most children can take either:
- Ibuprofen (Motrin/Advil): Best for swelling and inflammation. Use weight-based dosing every 6–8 hours as directed.
- Acetaminophen (Tylenol): Good for pain but doesn’t reduce swelling.
Always follow pediatric dosing guidelines. When in doubt, check with your Poppins care team, pediatrician, or pharmacist.
See Medications for Pain and Swelling for age-appropriate advice.
When Should I Follow Up With a Pediatrician?
Even with great home care, some injuries need follow-up.
Call your pediatrician if:
- Pain isn’t improving after 3–5 days.
- Your child can’t walk or use the limb at all.
- Pain is worsening despite rest and meds.
- Joint swelling or pain appears without any clear injury (could suggest infection or arthritis).
Poppins providers can help you decide next steps, from in-person exams to imaging.
See Follow-Up with Poppins for more on our approach.
Can My Child Return to Sports Right Away?
Short answer: Not until symptoms are gone.
- Wait until they’re symptom-free for 24–48 hours before returning to sports or high-impact play.
- Get an in-person assessment if you’re unsure.
- Watch for pain or limping with activity—and back off if symptoms return.
Pushing too soon risks re-injury, which can delay healing even more.
See When to Return to Sports and Activities for a safe plan.
We’ve Got You. Let’s Make Injuries Less Scary.
Parenting doesn’t come with an instruction manual, but you don’t have to figure this out alone. Poppins offers 24/7 access to pediatric care and personalized injury action plans—so you can care for your kid confidently. Sign up today and take the guesswork out of parenting care.

