Reviewed by: Alyson Insull, Pediatric Nurse Practitioner
One minute your kid looks fine, the next they’re covered in blotchy, bumpy welts—and you're deep in a frantic Google spiral about allergic reactions and emergency rooms. Sound familiar?
Hives in children can be alarming, but most of the time, they’re more annoying than dangerous. The key is knowing when to treat them at home, when to call your pediatrician, and when it’s time to escalate.
This guide breaks it all down so you can skip the guesswork, calm the chaos, and help your child feel better—fast.
What Are Hives (Urticaria) in Children?
Hives, also known as urticaria, are a common skin condition in children that often causes concern for parents. In fact, up to 25% of children will experience at least one episode of acute urticaria in their life.
These itchy, red or skin-colored welts can appear suddenly and may look alarming, but they are usually not dangerous. Understanding what hives look like, how they behave, and what they might mean can help you stay calm and take the right steps to care for your child.
What Do Hives Look Like in Kids?
Hives have some hallmark features that make them easier to recognize, even if the cause isn’t immediately clear. Here’s what to look for on your child’s skin:
- Raised, itchy welts or bumps (called wheals).
- Red or skin-colored, often with pale centers.
- Vary in shape and size (from pencil erasers to dinner plates).
- Come and go, sometimes lasting minutes or hours before moving to new areas.
- Blanch (turn white) when pressed.
In children with darker skin tones, redness may not be obvious. Instead, look for:
- Areas of swelling or puffiness.
- Warm patches on the skin.
- Subtle texture changes.
“In darker skin, hives can look more like subtle swellings than red patches,” says Aly Insull, a pediatric nurse practitioner at Poppins. “Feeling for warmth and texture changes can help.”
Summary: Hives are raised, itchy patches that change shape and location, and they may present differently depending on your child’s skin tone.
Common Causes of Hives in Kids
There are many reasons why your child might suddenly break out in hives.
From allergic reactions to infections, knowing the possible causes of pediatric hives can help you identify a pattern and avoid future flare-ups. Acute hives are typically short-lived and triggered by something specific, while chronic hives may persist for weeks without a clear cause.
Acute vs. Chronic Hives
Not all hives are the same—some are short-lived and easily linked to a trigger, while others stick around without a clear cause. While chronic hives are much less common, affecting only 1.8% of children, understanding the difference between acute and chronic hives can help guide treatment and determine when it’s time to see a specialist.
Here’s how they compare:
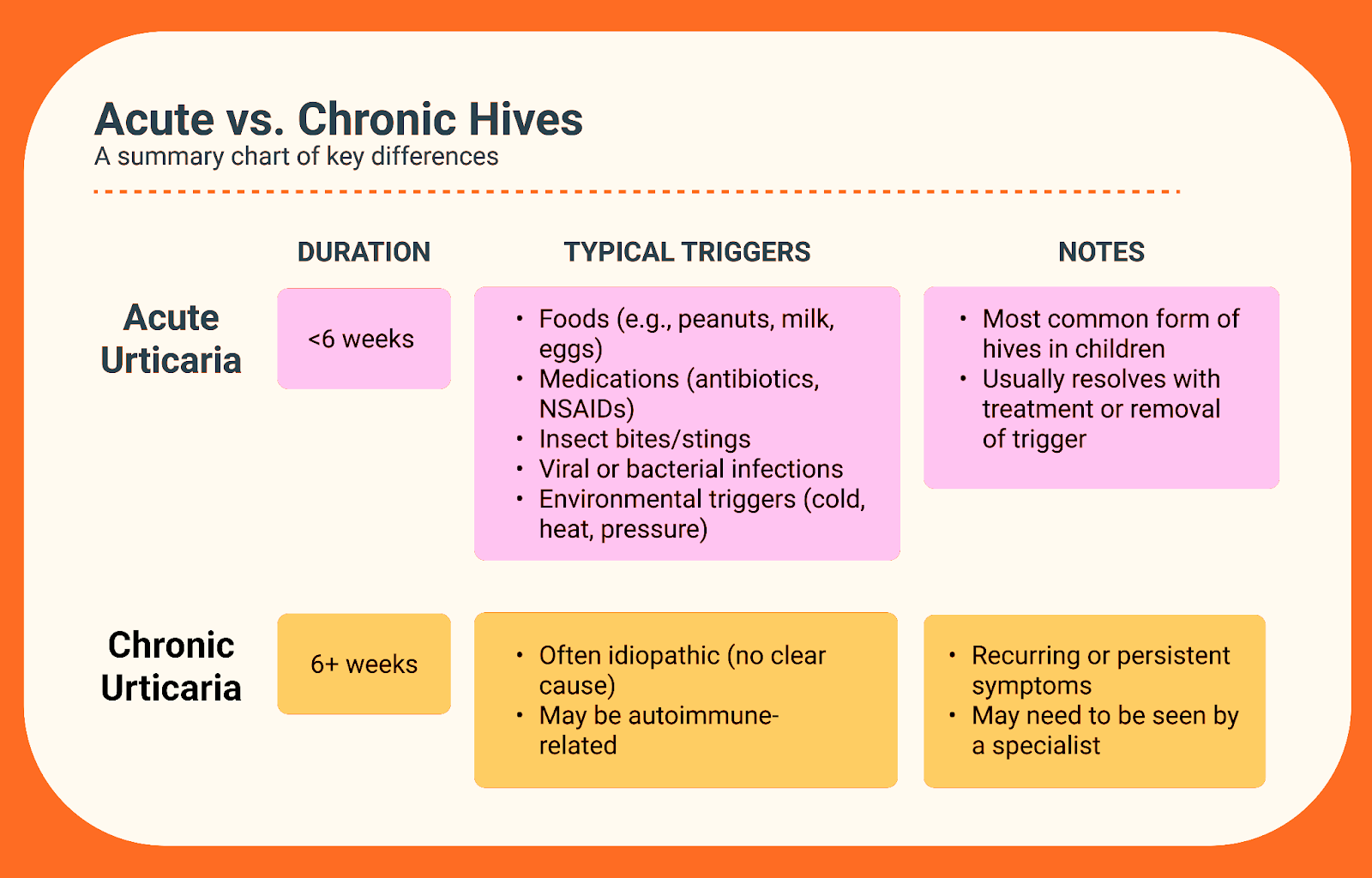
“If hives last more than six weeks, we start thinking about autoimmune causes or chronic idiopathic urticaria,” says Insull. “This is when a referral to an allergist or dermatologist may be helpful.”
Typical Triggers in Children
If your child suddenly breaks out in hives, one of these common triggers might be the culprit:
- Viral infections like colds or flu. Spoiler: viruses are responsible for nearly 50% of acute hive outbreaks in children under 5.
- New foods or snacks.
- Antibiotics, ibuprofen, or acetaminophen.
- Pet dander, dust mites, or pollen.
- Pressure from clothing or car seat straps.
- Exercise or changes in body temperature.
Summary: Hives can stem from a wide range of triggers, with acute cases tied to specific exposures and chronic hives often remaining unexplained.
Hives Symptoms to Watch For
Some are mild and fleeting, while others come with symptoms that signal a more serious problem. It’s important to recognize the signs that differentiate a benign rash from something that requires urgent medical attention. Tracking your child’s symptoms closely can help determine whether the hives are harmless or part of a larger issue.
Core Symptoms of Hives
Most cases of hives in children share a recognizable set of symptoms—here’s what to look for when evaluating your child’s rash:
- Itchy skin or rash.
- Raised, swollen welts that shift in location.
- Sometimes painful or burning.
- May be worse at night or after scratching.
Red Flag Symptoms
These symptoms require immediate medical attention:
- Difficulty breathing or swallowing.
- Swelling of the tongue, lips, eyes, or throat.
- Dizziness, fainting, or extreme fatigue.
- Nausea, vomiting, or stomach pain.
- Fever or joint pain.
“When hives are paired with breathing issues or swelling of the face, it could signal a more serious allergic reaction,” Insull notes. “Don’t wait—get medical help immediately.”
Summary: Hives are often mild, but systemic symptoms or signs of anaphylaxis require urgent care.
Questions to Help Identify the Cause
Identifying the trigger behind your child’s hives can help prevent future outbreaks and guide the best treatment. Medical professionals use targeted questions to assess whether the hives are related to a recent food, illness, medication, or environmental exposure. Gathering this history is a key part of diagnosing hives in kids.
Helpful Questions to Ask or Answer
To help identify what’s causing your child’s hives, consider these key questions that pediatric providers often ask during an evaluation:
- When did the hives first appear?
- Did your child eat a new food or take new medicine recently?
- Was your child sick or exposed to illness?
- Were they outdoors or bitten by insects?
- Do the hives appear in areas where clothes rub or where pressure is applied?
- Do the hives flare after heat, cold, exercise, or sun exposure?
- Are the hives coming and going for more than 6 weeks?
- Are there any patterns or obvious triggers?
“We ask parents to think back on meals, illnesses, and even laundry detergents,” says Insull. “Sometimes, the answer is in the little details.”
Bottom line: A thorough history is the best detective tool when it comes to identifying hive triggers in children.
How to Treat Hives in Kids
Many cases of hives in children can be safely and effectively managed at home with over-the-counter medications and simple skin care strategies. The goal is to relieve itching, reduce swelling, and prevent the rash from getting worse. Knowing which treatments are safe and effective for children is key.
First-Line Treatments for Acute Hives
Before you reach for the medicine cabinet, take a moment to look for any obvious triggers—like a new food, recent illness, or bug bite—and remove or avoid them if possible. Addressing the root cause is just as important as treating the symptoms.
Once triggers are removed, for most mild-to-moderate cases of hives in children, these go-to treatments can help reduce itching, calm inflammation, and speed up recovery:
- Non-drowsy antihistamines (safe for children)
- What they are: Daily oral allergy medications that block histamine, the chemical that causes hives.
- When they're used: First-line treatment to reduce itchiness and prevent new hives from forming.
- Safe for: Children 6 months and older (cetirizine); loratadine is typically used in children 2 years and up.
- Common options: Cetirizine or Loratadine at 0.25–0.5 mg/kg/dose, given once daily.
- Skin care
- What it includes: Soothing topical and bath-based treatments that help protect the skin barrier and relieve discomfort.
- When it’s used: Alongside antihistamines to calm irritated skin and reduce scratching.
- Best for: Children of all ages (use lukewarm water and gentle products).
- Examples:
- Oatmeal baths (DIY with colloidal oats or store-bought packets like Aveeno).
- Fragrance-free moisturizers (like CeraVe, Eucerin, or Vanicream).
- Cool compresses or lukewarm baths to relieve itching (important: avoid hot water).
- Topical treatments
- What it is: Over-the-counter steroid cream used on small patches of itchy skin.
- When it’s used: For localized hives that are particularly uncomfortable or persistent.
- Safe for: Children over 2 years (use sparingly and avoid broken skin).
- Common option: 1% Hydrocortisone cream applied 1–2 times daily for a few days.
Second-Line Treatment Options
If first-line treatments aren’t enough, your Poppins care team or pediatrician may recommend one of these second-line options to help manage more intense or widespread hives:
- Diphenhydramine (Benadryl)
- What it is: A sedating antihistamine that works quickly to relieve itching and swelling.
- When it's prescribed: Used for more severe or uncomfortable symptoms, especially when hives interfere with sleep.
- Safe for: Children 6 months and older (but often used cautiously due to drowsiness and shorter duration of action).
- Typical dose: 1–2 mg/kg/dose every 6 hours.
- Oral corticosteroids (e.g., Prednisolone)
- What it is: A short-course anti-inflammatory medication that reduces severe or widespread allergic reactions.
- When it's prescribed: Reserved for moderate to severe hives that are persistent, painful, or not improving with antihistamines.
- Safe for: Most children over 6 months, under medical supervision.
- Typical dose: 1–2 mg/kg/day (max 40 mg/day), usually for 3–5 days.
“Antihistamines are your first line of defense,” says Insull. “Cool baths and gentle skin care can also make a big difference in comfort.”
Summary: Most hives resolve with antihistamines, oatmeal baths, and moisturizers—but more intense cases may need additional medications.
How to Care for Your Children During a Hive Flare
When your child has hives, comfort and care go hand-in-hand. Alongside medication, lifestyle adjustments can help soothe itching, prevent skin damage, and keep your child from feeling miserable. Consistent home care can make a big difference in how quickly the rash resolves.
Home Care Tips for Hive Relief
Simple, soothing strategies at home can make a big difference in your child’s comfort during a hive flare:
- Avoid known or suspected triggers.
- Keep fingernails trimmed to prevent skin injury.
- Dress your child in soft, loose-fitting clothes.
- Use cool compresses on itchy spots.
- Avoid hot showers and baths, which can worsen symptoms.
Final thought: Supportive care is just as important as medication when helping your child feel better during a hives episode.
When Can My Child Go Back to School or Daycare?
It’s natural to wonder if your child’s hives mean they should stay home from school or daycare. The answer depends on the underlying cause of the rash and whether your child is otherwise well.
Understanding the guidelines can help you make a safe and informed decision.
Return Guidelines
Use these criteria to help you decide when it’s safe for your child to head back to school or daycare:
- No fever or systemic symptoms.
- Breathing is normal.
- Hives are improving or resolving.
- Child feels well enough to participate in regular activities.
“Hives alone aren’t contagious,” Insull says. “As long as the child feels okay and has no other symptoms, school or daycare is typically fine.”
Chronic Hives in Children: What to Know
If your child’s hives keep coming back or never fully go away, they may be dealing with chronic urticaria. This condition can be frustrating and mysterious, but with the right management plan, most kids can still live normal, active lives.
Here’s what to know about the long-haul version of hives in children.
Signs and Management of Chronic Hives
If your child’s hives stick around for weeks or keep coming back, here are the key signs that may indicate chronic urticaria:
- Hives persist or recur for more than 6 weeks.
- No identifiable trigger in many cases.
- Symptoms often respond to daily antihistamines.
- Specialist referral may be needed for autoimmune evaluation.
At-Home Strategies for Chronic Hives
To help manage chronic hives at home and reduce flare-ups, try the following parent-tested approaches:
- Keep a symptom diary (track food, weather, activities).
- Avoid known irritants (NSAIDs, stress, friction).
- Consider daily scheduled antihistamines.
“With chronic hives, families can feel really frustrated,” Insull acknowledges. “We help them build a sustainable care plan and coordinate with specialists if needed.”
Summary: Chronic hives take longer to resolve, but daily care and follow-up can help kids maintain a good quality of life.
When to Call the Doctor or Seek Emergency Care
While many hives cases are mild, some situations require professional medical attention. Knowing the red flags that indicate a serious allergic reaction or other underlying issue is crucial for keeping your child safe. Here’s how to know when to call your provider—or head to the ER.
Call a Pediatric Provider If:
Reach out to your Poppins care team or child’s pediatrician for further evaluation and guidance if any of the following apply:
- Hives last longer than 3 days.
- Symptoms worsen despite treatment.
- There’s no clear cause and hives keep recurring.
- New concerning symptoms appear
Go to the ER If:
Seek emergency care without delay if your child shows signs of a more serious allergic reaction, including:
- Child is having trouble breathing.
- There’s swelling of the tongue, lips, or throat.
- Symptoms include dizziness, vomiting, or fainting.
Summary: Keep an eye out for serious symptoms and don’t hesitate to seek help if your child’s condition changes or worsens.
Follow-Up with the Poppins Pediatric Team
At Poppins, follow-up care is part of the plan—not an afterthought. Our team is here to support your child’s recovery with personalized treatment plans, symptom monitoring, and 24/7 access to pediatric expertise.
Here’s what you can expect after your visit.
What Poppins Provides
- A written action plan and educational resources.
- A follow-up text within 24 hours.
- Guidance on when to reach out again.
- Escalation to specialists or ER if needed.
“Our goal is to make sure families feel supported and confident, not left guessing,” says Insull.
Summary: With Poppins, care doesn’t end when the visit ends—you’ll have support as long as you need it.
Frequently Asked Questions (FAQ)
Parents often have a lot of questions when their child breaks out in hives—and for good reason. Hives can show up suddenly, look dramatic, and make your child miserable, even if the cause is harmless.
Below are answers to some of the most common questions we hear from families.
Are Hives in Kids Contagious?
No, the hives themselves are not contagious. Urticaria is a skin reaction, not an infection. However, the underlying cause of the hives—such as a viral illness—can be contagious. For example, many viral infections that are common in childhood (like colds, hand-foot-and-mouth, or the flu) can trigger hives, especially in the early stages of illness.
If your child has hives but no fever, no respiratory symptoms, and seems otherwise well, they’re likely not contagious. But if the hives are part of a viral illness, you should monitor for additional symptoms and follow your pediatric provider’s return-to-school guidance. For more on this, see Hives Symptoms to Watch For and When Can My Child Go Back to School or Daycare?.
Are Hives in Kids Dangerous?
Most of the time, no. Hives in children are usually a short-term reaction to something like a viral illness, food, medication, or environmental trigger. They can look dramatic—and make your child pretty uncomfortable—but they’re often harmless and go away within a few days with the right care.
That said, hives can be dangerous if they’re accompanied by more serious symptoms like difficulty breathing, swelling of the face or throat, vomiting, or fainting. These may signal a severe allergic reaction (anaphylaxis) and require immediate medical attention.
To learn more about which symptoms are concerning, check out Hives Symptoms to Watch For and When to Call the Doctor or Seek Emergency Care. And for practical treatment tips, head to How to Treat Hives at Home.
How Long Do Hives Last in Children?
The duration of hives depends on the type and cause:
- Acute hives typically last anywhere from a few hours to 7 days. They may come and go throughout the day but should gradually improve.
- Chronic hives, defined as hives that persist or recur for more than 6 weeks, may not have an obvious trigger and often require a different approach to treatment and management.
If your child’s hives last beyond a week, don’t respond to antihistamines, or come back repeatedly, you may be dealing with chronic urticaria. Check out the Chronic Hives in Children section for a deeper dive into what to look for and when to seek specialist care.
Should I Give Benadryl for Hives?
Diphenhydramine (Benadryl) is a sedating antihistamine that can help reduce itchiness during a hive flare. However, newer antihistamines like cetirizine (Zyrtec) or loratadine (Claritin) are often preferred in children because:
- They’re non-sedating (won’t make your child drowsy or overly groggy).
- They offer longer-lasting relief.
- They have a better side effect profile for regular use.
“Antihistamines are the first line of defense for most hive episodes,” says Insull. “We usually recommend starting with non-sedating options unless symptoms are severe or interfering with sleep.”
If symptoms persist despite treatment, or if you’re unsure about dosing, consult your Poppins care team or pediatrician. You’ll find more dosing guidance in the How to Treat Hives in Kids section.
Can Teething Cause Hives?
No, teething does not directly cause hives. However, many babies develop drool rashes during teething—these can appear red, bumpy, and irritated, especially around the mouth and chin. While they might look like hives at first glance, drool rashes are more localized and not raised in the same way.
If your child develops a widespread rash, or the bumps appear in areas unrelated to teething (like the torso, arms, or legs), it’s more likely to be hives or another skin condition. When in doubt, compare the appearance of the rash to the examples in the What Are Hives (Urticaria) in Children? section or consult your provider.
What If My Child’s Hives Keep Coming Back?
If your child experiences repeated hive episodes, especially without a clear trigger, they may be experiencing chronic urticaria. While this condition is usually not dangerous, it can be uncomfortable and frustrating to manage. In these cases, your provider may recommend:
- Daily scheduled antihistamines.
- Keeping a symptom diary to track patterns or triggers.
- Referral to an allergist or dermatologist for further evaluation.
- Avoiding common irritants like NSAIDs, stress, heat, and tight clothing.
“Recurrent hives that linger beyond six weeks often fall under the chronic urticaria umbrella,” Insull explains. “It’s manageable, but it takes consistency and support.”
For more help, refer to the Chronic Hives in Children and Follow-Up with the Poppins Pediatric Team sections for next steps.

