Reviewed by: Alyson Insull, Pediatric Nurse Practitioner
One moment your child is happily finger-painting, the next they're scratching at a red, itchy rash—and you're wondering if it's something serious or just another mysterious kid skin thing.
Welcome to the confusing world of contact dermatitis.
In children, contact dermatitis is a common skin reaction that shows up when something irritates the skin or triggers an allergic response. In fact, up to 20% of children experience allergic contact dermatitis at some point in their lives. While it’s usually more uncomfortable than dangerous, figuring out what caused it—and how to help your child feel better—can be tricky.
This guide will walk you through what contact dermatitis looks like in kids, how to treat it, and when to get medical help (hint: Poppins is always here when you need us).
What Is Contact Dermatitis in Children?
Contact dermatitis is an inflammatory skin reaction that happens when your child’s skin touches something irritating or allergenic. It shows up as a rash that’s red, itchy, and sometimes scaly or blistered—and the location of the rash can be a big clue about the cause.
There are two main types:
- Irritant Contact Dermatitis (ICD): Caused by physical or chemical irritation (think soaps, wipes, or saliva). This is the most common type in kids.
- Allergic Contact Dermatitis (ACD): Triggered by an immune response to something your child is allergic to (like poison ivy, nickel, or certain cosmetics).
Both types can look similar, so understanding timing, exposure, and symptoms helps determine the type and best treatment.
What Does Contact Dermatitis Look Like in Kids?
A contact dermatitis rash can vary depending on your child’s skin tone, sensitivity, and the trigger. Here are some typical features:
- Red or pink rash on lighter skin; darker, purplish, or grayish patches on deeper skin tones.
- Itching or burning.
- Dry, cracked, or peeling skin.
- Bumps, blisters, or oozing (especially with allergic types).
- Rash shape matches area of contact (e.g., around the mouth from toothpaste or in a band shape from a bracelet).
Sometimes, you’ll notice your child is crankier than usual, scratching a lot, or not sleeping well because of the discomfort.
Common Causes of Contact Dermatitis in Children
Understanding what triggered your child’s rash is one of the most important steps in preventing future flare-ups. Contact dermatitis happens when the skin comes into direct contact with something that either irritates it or triggers an allergic immune response. While both types can look similar, their causes, timing, and treatment approaches differ.
Here’s a breakdown of the most frequent culprits in kids:
Irritant Contact Dermatitis (ICD) in Children
This is the most common type of contact dermatitis in children. It occurs when a substance physically damages or dries out the skin. It doesn’t require the presence of an allergy—any child can react, especially with repeated or prolonged exposure.
Common irritants include:
- Soaps and shampoos. Harsh or heavily fragranced soaps can strip the skin’s natural barrier, especially with frequent handwashing.
- Baby wipes and hand sanitizers. Alcohol-based sanitizers and preservative-laden wipes often cause dryness, stinging, or rash around sensitive areas like the diaper region or hands.
- Saliva (drool rash). Constant moisture from drooling—especially during teething—can break down skin around the mouth, chin, and neck.
- Detergents or cleaning products. Laundry detergents, dish soap, and all-purpose cleaners can irritate skin left in contact with residues on clothes or surfaces.
- Prolonged water exposure. Bathing too frequently or playing in water for extended periods can cause dry, cracked skin, particularly in children with sensitive skin.
Irritant dermatitis usually appears quickly—within minutes to a few hours of exposure. The rash often looks dry, red, or scaly and tends to stay limited to the area of direct contact.
“One of the most helpful things parents can do is retrace the 24 to 72 hours before the rash appeared. The answer is often hiding in plain sight—like a new soap or favorite bracelet,” says Aly Insull, a pediatric nurse practitioner at Poppins.
Allergic Contact Dermatitis (ACD) in Children
This type of dermatitis is caused by the immune system overreacting to a specific substance your child has developed a sensitivity to. These reactions are typically delayed, showing up 12 to 72 hours after contact with the allergen.
Common allergens in children include:
- Poison ivy, oak, or sumac. These plants contain urushiol oil, which can cause a red, blistering rash that often appears in streaks or patches on exposed skin.
- Nickel. Found in jewelry, belt buckles, snap buttons, zippers, and even cell phones. Nickel sensitivity is one of the most common causes of allergic rashes in kids with as many as 33% of children tested for nickel allergies experiencing positive reactions.
- Fragrance or preservatives in lotions, makeup, and sunscreen. Even products labeled “natural” can contain ingredients that cause allergic reactions—especially in children with eczema or sensitive skin.
- Latex. Present in balloons, gloves, pacifiers, and some medical supplies. Reactions can range from mild rash to more serious allergic symptoms in sensitive children.
- Adhesives in bandages or medical tape. Allergies to the sticky backing of bandages can cause localized rashes or blistering.
Quick Comparison: Irritant vs. Allergic Contact Dermatitis in Children
To help you quickly distinguish between the two types of contact dermatitis, here’s a side-by-side comparison of their most important features. This chart can be especially useful if you're trying to figure out whether your child’s rash is a fast reaction to irritation or a delayed allergic response.
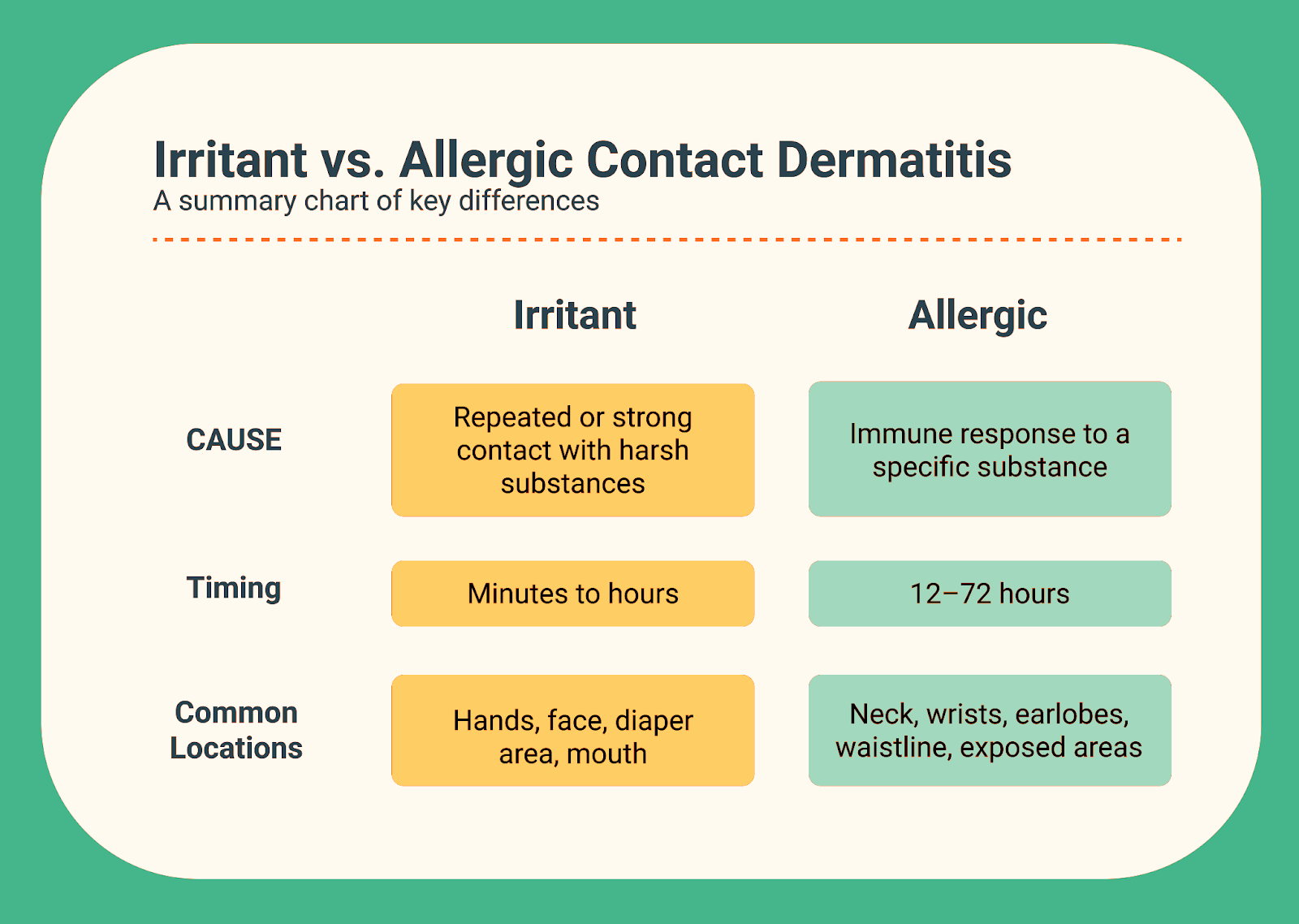
“If the rash shows up fast and looks dry or cracked, we think irritant. If it shows up later and looks blistered or angry, we start considering an allergic reaction,” says Insull.
Key takeaway: Irritant rashes tend to show up fast and improve with gentle care and avoidance, while allergic rashes are often delayed and may require more targeted treatment.
Symptoms of Contact Dermatitis in Kids to Watch For
Contact dermatitis can range from mildly irritating to downright miserable—but knowing how to recognize the signs can help you take action quickly and confidently.
In most cases, the rash is localized and improves with home care. But some symptoms may point to a more serious reaction or secondary infection that needs medical attention.
Here’s how to tell the difference:
Typical Symptoms of Contact Dermatitis
These are the most common signs of irritant or allergic contact dermatitis in children. They can vary depending on your child’s skin tone and sensitivity, but most cases share the following features:
- Itchy, red, or dry skin. A hallmark symptom—itching can range from mild to intense, often worse at night or with scratching.
- Swelling or puffiness. Mild swelling may occur around the rash, especially on thinner skin areas like the face or neck.
- Blisters or peeling skin. More common with allergic contact dermatitis (e.g., poison ivy), these may ooze or crust over as they heal.
- Clear pattern matching the source of contact. Look for rashes in defined shapes or lines—like under a wristband, around the mouth (from toothpaste), or in a diapered area.
If your child has these symptoms but is otherwise well—eating, playing, and sleeping normally—home care is usually appropriate.
More Serious Symptoms (Call Your Pediatrician or Poppins)
Some symptoms may indicate the rash is spreading, infected, or part of a more severe allergic reaction.
Call your provider or the Poppins care team if you notice:
- Rash spreading quickly or covering a large area of the body. Could suggest a more significant exposure, secondary reaction, or condition requiring additional treatment.
- Swelling near the eyes, lips, or face. These areas are more prone to complications. Swelling here may also indicate a more serious allergic response.
- Fever, fatigue, or reduced appetite. Systemic symptoms suggest the body is reacting to more than just a local skin irritant.
- Skin that’s hot, oozing pus, or smells bad. All potential signs of a skin infection. Infected dermatitis often requires antibiotics or prescription-strength treatments.
“If a rash is worsening or interfering with your child’s sleep, eating, or energy, it’s worth checking in with your care team,” recommends Insull.
Bottom line: If symptoms are staying mild and improving with home care, you're likely in the clear. But if your child seems unwell or the rash is progressing instead of resolving, don't wait—get in touch with your healthcare provider or a Poppins pediatric nursefor guidance.
Questions to Help Pinpoint the Cause
Here are some helpful questions parents can ask (or be prepared to answer) to help identify the trigger:
- When did the rash first appear?
- Did it start after using a new soap, wipe, or lotion?
- Is it in the shape or location of something that touched their skin?
- Did your child touch plants, pets, or new materials?
- Have they had this type of reaction before?
- Do they have eczema, asthma, or seasonal allergies?
- Have you tried any treatments? What worked (or didn’t)?
Sometimes, the tiniest detail—like switching laundry detergent—can be the answer.
How to Treat Contact Dermatitis at Home
Most cases of contact dermatitis can be managed at home with a few simple strategies. The goal: stop the reaction, soothe the skin, and prevent further irritation.
Step 1: Identify and Remove the Trigger
Before you reach for creams or medications, the most important step is to stop the exposure that’s causing the reaction. Whether it’s a new lotion, a household cleaner, or a plant your child brushed up against, identifying and eliminating the trigger can prevent the rash from getting worse—and keep it from coming back.
Start with these essential first steps:
- Wash the affected skin with mild soap and lukewarm water as soon as possible after contact. This helps remove any remaining irritant or allergen from the surface of the skin.
- If your child’s rash was caused by a plant like poison ivy, oak, or sumac, be thorough:
- Wash all clothing, towels, shoes, and other items that may have come into contact with the plant oil (urushiol).
- Don’t forget about pets—plant oils can cling to fur, and touching a contaminated pet can trigger another reaction.
Catching and removing the trigger early can dramatically shorten the duration of the rash and reduce the severity of symptoms.
Step 2: Soothe the Skin
Once you’ve removed the trigger (or narrowed it down), the next step is helping your child feel better.
Contact dermatitis can be itchy, dry, and uncomfortable—especially for kids who can’t stop scratching. The right skin care routine can make a big difference in healing, prevent further irritation, and reduce the risk of infection.
Focus on gentle, consistent care using these strategies:
- Moisturize regularly with fragrance-free products to repair the skin barrier and lock in hydration:
- Lotions/Creams: CeraVe, Cetaphil, Vanicream, Eucerin, Aveeno.
- Ointments: Aquaphor, Vaseline, CeraVe Healing Ointment.
- Cool compresses: Apply a soft, damp washcloth to itchy areas or let your child soak in cool water for 20 minutes every few hours as needed.
- Avoid hot baths or showers, which can dry out and further irritate already inflamed skin.
- Trim fingernails to reduce the chance of scratching open the skin, which can lead to infection.
This doesn’t have to be complicated. Think: simple products, gentle care, and regular routines. A little consistency goes a long way in helping your child’s skin heal.
“Most contact dermatitis in kids can be handled at home with gentle skincare, cool compresses, and avoiding whatever caused the reaction. You don’t need a cabinet full of products—just the right ones,” advises Insull.
Step 3: Medications
In many cases, medication can help relieve itching, reduce inflammation, and speed healing—especially if the rash is causing discomfort or interfering with sleep. Below are the most commonly used treatments for contact dermatitis in children.
Hydrocortisone Cream (1% or 2.5%)
- What it is: A topical corticosteroid that reduces inflammation, redness, and itching.
- What it’s used for: Short-term treatment of irritated, inflamed, or itchy skin caused by allergic or irritant contact dermatitis.
- Safe for: Children over 2 years old. Use with caution in infants and only under medical supervision.
- Application guidelines:
- Use 1% strength on sensitive areas like the face, groin, or underarms.
- Use 2.5% strength on less sensitive areas like the arms, legs, or torso.
- Apply a thin layer to affected areas twice daily for up to 7 days.
- Note: Do not use on broken skin. If symptoms haven’t improved after a week, contact your provider for reassessment.
“Steroid creams help reduce inflammation, but they're less effective if the cause is an irritant rather than an allergen,” warns Insull.
Oral Antihistamines: Cetirizine (Zyrtec) or Diphenhydramine (Benadryl)
- What they are: Medications that block histamine, the chemical that triggers allergic responses like itching and swelling.
- What they’re used for: Reducing itchiness and discomfort from allergic skin reactions, especially if symptoms are disrupting sleep.
- Safe for:
- Cetirizine (Zyrtec): Children 6 months and older.
- Diphenhydramine (Benadryl): Children over 6 months, used with caution due to sedating effects.
- Dosage guidelines:
- Cetirizine: 0.25–0.5 mg/kg/dose, given once daily.
- Diphenhydramine: 1–2 mg/kg/dose every 6 hours, as needed. Use primarily at night due to drowsiness.
- Note: Always confirm dosage with your Poppins care team or pediatric provider, especially for infants or younger children.
Reminder: These medications provide relief but don’t address the root cause. For lasting improvement, it’s essential to identify and avoid the trigger.
Chronic or Recurrent Rashes: What’s Next?
If your child keeps getting rashes in the same area, they may be experiencing repeated contact with the same trigger—or they could have a related condition like eczema, which occurs in 1 out of every 10 kids. Keeping a symptom diary and reviewing product ingredients can help narrow things down.
Your care team may recommend:
- Referral to an allergist or dermatologist.
- Allergen patch testing.
- Daily preventive skincare routine.
When Can My Child Go Back to School or Daycare?
In most cases, contact dermatitis isn't contagious and kids can return to school when:
- The rash is not oozing or draining.
- There are no systemic symptoms like fever.
- They feel well enough to participate in normal activities.
If the rash is actively oozing, it’s best to keep your child home until the skin is dry and healing.
When to Call the Doctor (or Poppins)
Most cases of contact dermatitis in children can be treated at home—but sometimes a rash is more than just a rash. If your child’s symptoms are worsening, aren’t responding to treatment, or you’re unsure about what’s causing the reaction, it’s time to get expert support.
Here’s when to reach out to your pediatric provider or your Poppins care team for additional evaluation and treatment:
Call your pediatrician or Poppins if:
- The rash is spreading, worsening, or not healing after 7 days of home treatment.
- Your child develops a fever, fatigue, or other signs of systemic illness.
- The rash appears near the eyes, lips, or genitals, where skin is more delicate and complications are more likely.
- There are signs of possible skin infection, such as:
- Yellow or green drainage.
- Skin that feels warm or firm to the touch.
- Increasing redness or swelling.
- A bad smell coming from the rash.
- You’re not sure what caused the rash or whether your current treatment is safe or effective.
- The rash keeps coming back, and you suspect a recurring allergen or chronic skin condition.
Seek emergency care immediately if:
- Your child is having trouble breathing or swallowing.
- There is sudden or severe swelling of the face, lips, eyes, or throat.
- The rash turns into large blisters (bullae) or spreads quickly over a large area of the body.
- Your child shows signs of a severe allergic reaction (anaphylaxis), including fainting, vomiting, or a dramatic drop in energy or responsiveness.
“If the rash is spreading fast, near the eyes, or making your child truly miserable, that’s a good time to check in. We’d always rather you ask than wait it out,” advises Insull.
Bottom line: If your gut says something isn’t right—or if your child’s condition is getting worse instead of better—it’s always better to check in. Poppins offers 24/7 access to pediatric expertise, so you don’t have to make that call alone. We're here to guide you from the first rash to full recovery.
Poppins Care for Contact Dermatitis in Kids
You don’t have to figure this out alone. When your child has a rash, we’re here to help you get answers, relief, and a plan—fast. Here’s what you can expect when you reach out to Poppins:
- A personalized treatment plan that includes home care instructions, medication guidance, and clear steps tailored to your child’s symptoms and skin type.
- A follow-up text within 24 hours to check how your child is doing, adjust the plan if needed, and answer any new questions you have.
- Support identifying potential irritants or allergens, including help reviewing soaps, lotions, wipes, detergents, and other everyday products.
- Guidance on when to escalate care, whether that means a referral to a specialist, a prescription, or an ER visit if red flag symptoms develop.
- Ongoing support from a trusted pediatric team, available 24/7 for questions, flare-ups, and follow-up—even if it’s your third rash of the month.
Bottom line: With Poppins, you’re never left guessing. We make sure you have the expert support, follow-up care, and real-time guidance you need—right when you need it.
FAQ: Parents’ Top Questions About Contact Dermatitis
When your child breaks out in a rash, it’s completely normal to have a lot of questions. These are some of the most common concerns we hear from parents navigating contact dermatitis.
Is Contact Dermatitis Contagious?
No—contact dermatitis is not contagious. It’s a skin reaction to an irritant or allergen, not a bacterial or viral infection. That means your child can’t “give” the rash to anyone else.
However, if the affected skin becomes infected—for example, from scratching open blisters or scabs—bacteria can spread and require treatment. In those cases, you may notice oozing, a foul smell, or increased redness and warmth. Learn more about when to call the doctor in the When to Call the Doctor section.
How Long Does Contact Dermatitis Last in Children?
The duration of contact dermatitis depends on the type, cause, and how quickly it’s treated:
- Irritant contact dermatitis typically improves within a few days and clears up in 1–2 weeks once the trigger is removed and proper skin care is started.
- Allergic contact dermatitis may last longer—up to 2–3 weeks—especially if the exposure continues unknowingly (e.g., nickel in clothing fasteners or hidden fragrances in skincare).
If the rash persists longer than 3 weeks, worsens, or keeps coming back, reach out to your provider. For detailed care tips, visit the How to Treat Contact Dermatitis at Home section.
What Can Be Mistaken for Contact Dermatitis?
Allergic skin conditions are very common in children with nearly 9 million reported cases annually. Several childhood skin conditions can look similar to contact dermatitis, especially in the early stages.
Common lookalikes include:
- Eczema (atopic dermatitis): Often chronic, dry, and itchy, but not triggered by a specific contact. It typically appears on cheeks, arms, or behind knees.
- Fungal infections (like ringworm): Can start as a red, itchy patch with a raised border. These often grow slowly in size and may have central clearing.
- Viral rashes (e.g., hand-foot-and-mouth disease): Typically accompanied by fever and other systemic symptoms.
- Heat rash (miliaria): Small, red bumps caused by blocked sweat glands, often in warm or humid conditions.
If the rash doesn’t improve with typical contact dermatitis treatments, spreads unexpectedly, or is accompanied by fever or behavior changes, it’s a good idea to consult your Poppins care team or pediatrician. Visit the Symptoms to Watch For section for more guidance on when to seek help.
What is The Fastest Way to Heal Contact Dermatitis?
The quickest way to heal contact dermatitis in kids is a combination of trigger removal, skin protection, and symptom relief:
- Identify and remove the cause as soon as possible. Even low-level exposure can keep the rash going. See Step 1: Identify and Remove the Trigger.
- Soothe the skin with fragrance-free moisturizers and cool compresses. Reapply creams often to support the skin barrier. See Step 2: Soothe the Skin.
- Use medications as directed, such as low-dose topical steroids and antihistamines to reduce inflammation and itch. See Step 3: Medications.
- Prevent scratching to avoid skin damage and infection—keep nails short and use soft fabrics.
With consistent care, most cases improve noticeably within 48–72 hours and clear within a week. If not, it’s time to check in with your pediatric provider.
Should I give Benadryl or Zyrtec for my child’s rash?
Both Benadryl (diphenhydramine) and Zyrtec (cetirizine) are antihistamines that can help relieve itchy skin and discomfort from contact dermatitis. Here’s how they compare:
- Zyrtec is a non-drowsy antihistamine that works well for ongoing itching and is better suited for daytime use and longer-term relief.
- Benadryl works faster but can cause drowsiness and may wear off more quickly—often used at night or for more intense flares.
Most pediatric providers prefer Zyrtec for daytime itching due to its longer-lasting and gentler side effect profile. Dosing depends on your child’s age and weight—always check with your Poppins care team or provider for guidance.

